Article
COVID-19 Continues to Result in High Admission, Fatality Rates Among Patients With CLL
Author(s):
COVID-19 continued to result in high admission and fatality rates among patients with chronic lymphocytic leukemia during the first 13 months of the pandemic, and although risk of severe infection was determined to be independent of age, CLL status, and treatment, being age 75 years or older was revealed to be a significant risk factor for death.
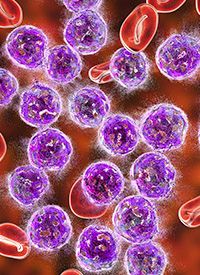
COVID-19 continued to result in high admission and fatality rates among patients with chronic lymphocytic leukemia (CLL) during the first 13 months of the pandemic, and although risk of severe infection was determined to be independent of age, CLL status, and treatment, being age 75 years or older was revealed to be a significant risk factor for death, according to data from a poster presented during the 2021 International Workshop on CLL.1
Results from the analysis showed that 77% (n = 46) of 60 patients were hospitalized because of severe infection with the virus, and 24% (n = 11) of patients were admitted to the intensive care unit (ICU). Severe infection was found to be equally distributed across patient subgroups, including age, gender, body mass index (BMI), CLL status, and CLL treatment; however, this was not true for Cumulative Illness Rating Scale (CIRS) score (P < .05).
Twenty-three percent of patients (n = 14) died, but an age of 75 years or older was determined to be the only significant risk factor for death (P < .05 on multivariate analysis).
Moreover, when comparing outcomes between months 1 through 6 and months 7 through 13, the rate of ICU admission dropped from 37% to 15%, as did the death rate, going from 32% to 18%. However, admissions to the hospital continued to be frequent in both time periods, at 86% and 71%, respectively.
In both periods, 85% of patients who were admitted to the hospital required supplemental oxygen. From the first time period to the second, the use of remdesivir (Veklury) increased from 5% to 41%, and the use of corticosteroids also increased, going from 47% to 78%.
“Risk of death and ICU admission declined in the second time period,” lead study author Lisa Blixt, of Department of Hematology at Karolinska Hospital Solna and the Department of Oncology/Pathology at Karolinska Institut, and colleagues, wrote in the poster on the data. “A robust and durable B- and/or T-cell immunity was observed in most convalescents.”
Patients with CLL are known to be at greater risk for severe infections because of disease- and treatment-related immunodeficiency. During the COVID-19 pandemic, data from international surveys conducted earlier on revealed a high fatality rate among those with this disease who were admitted to a hospital because of a severe infection with COVID-19. It is also known that this patient population might not adequately respond to vaccination against the virus.
In the analysis shared during the meeting, investigators shed light on the clinical and immunological outcomes of COVID-19 in consecutive patients with CLL from a well-defined area during the first 13 months of the pandemic.
The objective of the research was to evaluate hospitalization, ICU admissions, and fatality rates in 2 time periods during the pandemic: months 1 to 6 and months 7 to 13. By doing these, they hoped to determine potential prognostic factors for patients. They also wanted to examine B- and T-cell immunity during long-term follow-up.
The analysis included 60 patients with CLL who were at 3 hematology centers in Stockholm. These patients had a history of polymerase chain reaction–confirmed, symptomatic COVID-19 between March 1, 2020 and March 31, 2021.
The median age of these patients was 71 years (range, 43-97) with 32% of patients aged 75 years and older, and 65% of patients were male. The median CIRS was 8 (range, 4-20), with 75% of patients having a CIRS of greater than 6. The median BMI was 25 (range, 19-42), 30% had diabetes, 53% were never smokers, and the median IgG was 7.9 g/L (range, 2.1-13.4).
At the time of their COVID-19 diagnosis, 63% were never treated with treatment for their CLL, 20% were previously treated, and 17% continued to receive treatment. Of those receiving ongoing treatment, 70% were on a BTK inhibitor. Regarding disease status at the time of their COVID-19 diagnosis, 63% had stable disease, 25% were in complete response or partial response, and 12% had experienced progressive disease.
Investigators collected information on COVID-19 symptoms, hospitalization or ICU attendance and the duration of the stay, treatment for COVID-19, and clinical outcome. Convalescent blood samples were also taken from most patients at 3 to 6 months and up to 1 year after infection; these samples were evaluated for SARS-CoV-2 antibodies.
Immunological analyses were also conducted in a subset of convalescents to examine whether antibodies were able to neutralize, whether SARS-CoV-2–specific antibodies could be detected in saliva, and whether patients experienced T-cell immune responses.
These analyses revealed that 83% of 41 convalescents experienced seroconversion. Antibodies continued to be identified at 6 months in 17 of 22 patients; they remained detectable at 12 months in 8 of 11 patients. Moreover, 13 of 17 patients were found to have neutralizing antibodies; however, 1 patient was negative in conventional serology.
Notably, SARS-CoV-2–specific T cells were identified in 82% of 17 patients and were noted to be paralleled by seroconversion, overall.
Reference
- Blixt L, Bogdanovic G, Buggert M, et al. Covid-19 in patients with chronic lymphocytic leukemia: clinical outcome and B- and T-cell immunity during 13 months in consecutive patients. Presented at: 2021 International Workshop on CLL; September 17-20, 2021; virtual. Poster 1084244. https://bit.ly/3zlCyCb








