News
Article
Relma-Cel Continues to Elicit Responses in Chinese Patients With R/R Mantle Cell Lymphoma
Author(s):
Relmacabtagene autoleucel continued to induce responses with acceptable tolerability in Chinese patients with relapsed or refractory mantle cell lymphoma.
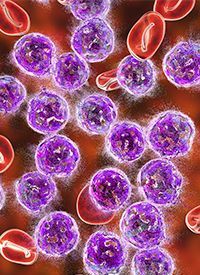
Image Credit: ©Dr_Microbe - stock.adobe.com
Relmacabtagene autoleucel (relma-cel; Carteyva) continued to induce responses with acceptable tolerability in Chinese patients with relapsed or refractory mantle cell lymphoma (MCL), according to updated data from an open-label phase 2 study (NCT04718883) presented at the 2023 ASH Annual Meeting.1
At month 3, the objective response rate (ORR) achieved with the CD19-directed CAR T-cell therapy was 64.29% (95% CI, 48.03%-78.45%), with a complete response (CR) rate of 54.76% (95% CI, 38.67%-70.15%) in efficacy-evaluable patients (n = 42). The best ORR with relma-cel was 78.57% (95% CI, 63.19%-89.70%), with a best CR rate of 66.67% (95% CI, 50.45%-80.43%).
“Given the poor baseline characteristics of the MCL patients, relma-cel still demonstrated high response rates and good tolerability for the treatment of relapsed/refractory MCL,” Yuqin Song, MD, PhD, of the Department of Lymphoma, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education) at Peking University Cancer Hospital & Institute in Beijing, China, and colleagues, wrote in a poster.
The median overall survival (OS) of patients with mantle cell lymphoma is about 3 to 4 years from diagnosis. This population is known to achieve poor responses with available treatment and experience high rates of recurrence. Those who have progressed on BTK inhibitors have been shown to achieve a best ORR of about 27% and a median OS ranging from 6 to 10 months.
The phase 2 study included patients with a confirmed MCL who had relapsed or refractory disease. Patients had previously received an anti-CD20 antibody, anthracycline, or bendamustine (Bendeka), and a BTK inhibitor.
Study participants first received lymphodepletion chemotherapy and then were administered relma-cel at 100 x 106 CAR+ T cells. Those who received bridging therapy were required to have a washout period. The primary end point of the trial was 3-month ORR, and secondary end points comprised 3-month CR rate, duration of response, progression-free survival, OS, pharmacokinetics, pharmacodynamics, and safety.
As of the data cutoff date of June 30, 2023, a total of 66 patients had been enrolled and undergone leukapheresis. The CAR T-cell therapy was given to 56 patients, 42 of whom had 3 months of follow-up or had discontinued treatment because of disease progression or death prior to assessment.
In the 56 patients who received the CAR T-cell therapy, the median age was 59.5 years (range, 34-75), with 66.1% of patients under 65 years. Most patients were male (78.6%), and more than half had an ECOG performance status of 1a or higher (57.1%). Additionally, 46.4% had relapsed disease, 50.0% were refractory, 1.8% were uncategorized, and 1.8% had missing information. Moreover, 23.2% had blastoid histology and 10.7% had pleomorphic variants.
Additionally, 1.8% previously received 1 line of systemic treatment, 30.4% had 2 prior lines, 41.1% had 3 to 4 lines, 25.0% had 5 or more prior lines, and 1.8% had missing information. Just over half of patients had relapsed on a BTK inhibitor (55.4%) and 44.6% were refractory to this agent. The sum of the perpendicular diameters was up to 8000 mm2 for 89.3% of patients. In terms of bulky disease, 30.4% had disease that was at least 5 cm, 21.4% had disease less than 10 cm, 8.9% had disease that was 10 cm or larger, and 69.6% had disease that was less than 5 cm.
Mantle Cell Lymphoma International Prognostic Index score was 0 to 3 for 50.0% of patients, 4 to 5 for 32.1% of patients, and 6 to 11 for 16.1% of patients; this information was missing for 1.8% of patients. Additionally, 12.5% had relapsed after hematopoietic stem cell transplantation. About half of patients (53.6%) had an extranodal lesion; 30.4% had bone marrow involvement, 7.1% had gastrointestinal involvement, and 50.0% had spleen involvement. Just under half of patients (46.4%) received bridging therapy, 34.6% of whom required high-intensity chemotherapy to control progressive disease.
Any-grade adverse effects (AEs) occurred in 98.21% of safety-evaluable patients (n = 56); any-grade treatment-emergent AEs (TEAEs) were reported in 92.86% of patients. Grade 3 or higher TEAEs occurred in 85.71% of patients. Moreover, treatment-related TEAEs were observed in 92.86% of patients; these effects were grade 3 or higher for 78.57% of patients.
Any-grade cytokine release syndrome (CRS) was reported in 55.36% of patients; this was grade 3 or higher for 5.36% of patients. Any-grade and grade 3 or higher neurotoxicity was experienced by 10.71% and 7.14% of patients, respectively. Most patients experienced prolonged cytopenia (83.93%); these effects were grade 3 or higher for 67.86% of patients. Infections and infestations occurred in 48.21% of patients, with grade 3 or higher effects reported in 26.79% of patients.
Serious AEs were reported in 44.64% of patients. SAEs related to the CAR T-cell therapy occurred in 23.21% of patients. Eighteen patients died, with 2 deaths determined to be related to treatment; these patients experienced pneumonia or multiorgan failure.
Reference
- Song Y, Zhou K, Li L, et al. Safety and efficacy of Relmacabtagene autoleucel (relma-cel) in adults with relapsed/refractory mantle cell lymphoma (r/r MCL): updated results from a phase II open-label study in China. Blood. 2023;142(suppl 1):3024. doi:10.1182/blood-2023-178430








