Article
European Panel Recommends Against Neratinib for HER2-Positive Breast Cancer
Author(s):
European regulators have recommended against approving a marketing authorization application for the use of neratinib (Nerlynx) as extended adjuvant treatment for women with early stage HER2-positive breast cancer.
breast cancer
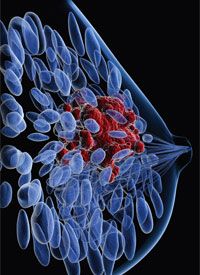
European regulators have recommended against approving a marketing authorization application (MAA) for the use of neratinib (Nerlynx) as extended adjuvant treatment for women with early stage HER2-positive breast cancer.
In January, the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency informed Puma, the manufacturer of neratinib, about a negative trend vote following a meeting to discuss the MAA. The negative CHMP opinion will be sent to the European Commission for a final regulatory decision. Puma announced in a press release that it plans to request a re-examination of the opinion.
The CHMP based its vote on data from the phase III ExteNET and phase II CONTROL trials, which were the same studies the FDA considered when approving neratinib in this setting last year.
Five-year follow-up data from ExteNET published in late 2017 in the Lancet Oncology showed that in women with HER2-positive stage I to IIIc operable breast cancer, extended adjuvant therapy with neratinib reduced the risk of invasive disease recurrence or death by 27% compared with placebo when given following 12 months of trastuzumab (Herceptin).
The 5-year invasive disease-free survival (DFS) rate with neratinib was 90.2% (95% CI, 88.3-91.8) compared with 87.7% (95% CI, 85.7-89.4) with placebo. After a median follow-up of 5.2 years (IQR, 2.1-5.3), patients in the neratinib group had 116 invasive disease-free survival (DFS) events compared with 163 for those in the placebo group (HR; 0.73; 95% CI, 0.57-0.92; P = .0083).
The restricted mean invasive DFS was 56.5 months (95% CI, 55.9-57.2) in the neratinib group (mean loss of 3.5 months from a total of 60 months) compared with 55.2 months (95% CI, 54.4-55.9) in the placebo group (mean loss of 4.8 months from a total of 60 months). The between group difference was 1.3 months (95% CI, 0.3-2.3; P = .0085).
The 5-year analysis was not originally planned as part of the study and was requested as part of a new drug application for neratinib in the United States and for an MAA in Europe. The primary endpoint of the study was the 2-year invasive DFS rate, which was 93.9% with neratinib and 91.6% with placebo (HR, 0.67; P = .009)
In the phase III study, 2840 patients who remained disease-free following 1 year of treatment with adjuvant trastuzumab and chemotherapy were randomized to neratinib (n = 1420) or placebo (n = 1420). The interval between receiving trastuzumab and entering the trial was approximately 4.5 months. Patients received 240 mg of neratinib daily or placebo for 12 months.
The median age of patients in the study was 52 years and approximately 23.8% had node-negative disease, with 46.6% of patients having 1 to 3 positive nodes and 29.6% having ≥4 positive nodes. Anthracyclines were administered as adjuvant chemotherapy in the majority of patients (77%). Appropriate endocrine therapy was administered to 94% of patients with HR-positive breast cancer.
The safety population included 2816 patients who received at least one dose of study treatment, 1408 patients in each group. The primary safety analysis was reported at the 2year follow-up, but investigators saw no evidence of long-term toxicity in these updated findings.
Across the full study population, 95.4% of patients treated with neratinib experienced all-grade diarrhea, of which 40% was grade 3/4. The trial design did not mandate antidiarrhea prophylaxis.
Other gastrointestinal-related adverse events included nausea (43%), fatigue (27%), vomiting (26%), and abdominal pain (24%). In the placebo arm, 36% of patients had all-grade diarrhea, with a grade 3/4 incidence of 2.0%.
Although patients in the ExteNET study were not required to receive antidiarrheal prophylaxis, the ongoing, open-label phase II CONTROL trial examined the preventative measure in HER2-positive patients who received neratinib for 1 year along with antidiarrheal prophylaxis given during the first two 28-day treatment cycles.
At the data cutoff, 137 patients had received prophylaxis with loperamide alone, 64 patients had received loperamide plus budesonide, and 26 patients had received loperamide plus colestipol. The median duration of neratinib treatment for the 3 cohorts was 10.6 months, 5.1 months, and 1.7 months, respectively.
Comparing the loperamide-alone CONTROL cohort to the safety data cohort from the ExteNET trial (n = 1408), the incidence of all-grade diarrhea was 77.4% versus 95.4%, respectively. The rates of grade 3 diarrhea were 30.7% versus 39.8%, respectively.
The rate of dose reductions (7.3% vs 26.4%) and holds (14.6% vs 33.9%) due to diarrhea were lower in the patients who received loperamide. However, the rate of discontinuation due to diarrhea was higher in the loperamide cohort at 20.4% versus 16.8% with neratinib alone.
References
- Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab-based adjuvant therapy in HER2-positive breast cancer (ExteNET): 5-year analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017; 18:1688-700.
- Puma Biotechnology presents interim results of phase II CONTROL Trial of PB272 in extended adjuvant treatment of her2-positive early stage breast cancer at the 2017 AACR Annual Meeting. Posted April 4, 2017. Accessed February 23, 2018. http://bit.ly/2EXiduL.







