Publication
Article
Hotspot ESR1 Mutations Drive Tumor Stickiness in Metastatic Endocrine-Resistant Breast Cancer
Author(s):
The prevalence of ESR1 mutations in endocrine-resistant metastatic breast cancer has paved an avenue for investigators to explore their role in the promotion of metastasis.
Steffi Oesterreich, phd

The prevalence of ESR1 mutations in endocrine-resistant metastatic breast cancer has paved an avenue for investigators to explore their role in the promotion of metastasis. ESR1 mutations have been reported in 20% to 40% of patients who received endocrine therapy with aromatase inhibitors (AIs), particularly in those who received therapy in the metastatic setting.1,2
Recent efforts have unpacked the role of somatic mutations to trigger metastatic phenotypes pulling 2 distinct hotspot mutations into focus—Y537S and D538G. Two articles recently published in Cancer Research and Nature Communications respectively unpack the previously unexplored role of ESR1 in metastatic disease progression and the association of these mutations with immune activation.3,4
“Our study provides a resource for other groups to mine the data from the cell line, from the mouse models, and from tumors,” said lead study author Steffi Oesterreich, PhD, in an interview with OncologyLive®. “Others can get access to the data, see [whether] they find something, and use the ideas for that. [It is] always very important to have it as a resource for other groups interested in an ESR1-mutant and endocrine-resistant tumors.”
Early efforts to model ESR1-mutant disease in with endocrine resistance resulted in the conclusion that ESR1 mutants had context- and mutation-specific features.5 The team of investigators used the foundational insights from examining Y537S and D538G to further classify gain-of-function metastatic characteristics that may be triggered by somatic ESR1 muations.3,5
Prevelance of Hotspot Mutations
Investigators began with an analysis of the broad genomic events observed across cohorts of patients with metastatic breast cancer to identify commonalities among patients with ESR1-mutant disease. Frequency of ESR1 mutations were compared between distant metastases and locally recurrent tumors in 2 analyses. The first analysis included compiled data from 4 cohorts of previously reported studies, which showed that among 877 distant metastases, 18% harbored ESR1 mutations, and among 44 local recurrences, no tumor samples had ESR1 mutations.3
An additional 75 recurrent tumor samples from the Women’s Cancer Research Center and the Charité Hospital in Berlin, Germany, were assessed for ESR1 mutation status using droplet digital polymerase chain reaction analysis targeting Y537S and D538G hotspot mutations. Similar to the observations of the compiled studies, mutations were identified in 25% of the distant metastases and in none of the local recurrences.3
In this analysis, investigators also noted that ESR1 mutations were more prevalent among those who had received more prior lines of therapy compared with those who had wildtype disease. Further, in a meta-analysis of all samples, Y537S and D538G variant mutations were reported in 37% and 24% of tumors, respectively.3
Tumor Cell ‘Stickiness’
Following confirmation of the prevalence of ESR1 mutations in metastatic tumors, investigators evaluated mutant cell models to unpack the mechanistic behaviors of cells. Investigators looked to cell-cell interaction as a driver of metastases and observed that ESR1-mutant cell lines had a prevalence of mutant cells aggregating together in clusters of 5 or more cells.3 Based on these findings, circulating tumor cell (CTC) clusters were examined for gene signatures in ESR1-mutant tumors. Compact cell clustering and faster aggregation of cells were reported in 2 mutant cell lines—MCF7 and T47D—specifically in MCF7/Y537S, MCF7/ D538G, and T47D/Y537S cells.3
“These results show that hotspot ESR1 mutations confer increased cell-cell attachment under static and fluidic conditions, and the effect size is dependent on mutation type and genetic backgrounds,” the study authors wrote.3
Investigators next sought to build a CTC cluster gene signature based on an expression analysis from patients with estrogen receptor–positive disease with at least 2 CTC clusters. When applied to a sample of 51 metastatic tumors via RNA sequencing, investigators observed correlation of higher enrichment of CTC cluster gene signatures present in ESR1-mutant metastatic tumors.3
Finally, to examine the effect of clustering of CTCs on clinical outcomes, an analysis of ESR1-mutant tumors from 151 patients with metastatic breast cancer was performed. Clusters were detectable in 14 patients, with a median number of 15.5 (interquartile range, 4-20) cells per cluster. Patients were stratified by CTCs greater than 4 per cluster (n = 10) and fewer than or equal to 4 cells per cluster (n = 4). In terms of prognosis, patients with stage IV indolent disease who had more than 4 clustered CTCs had worse prognosis compared with those who had fewer than 4 clustered CTCs in both in the overall population (P < .0001) and in the estrogen receptor–positive/HER2-negative subgroup (P < .00001).3
In addition to the clustering CTCs, investigators noted that gap junction and desmosome genes are also more prevalent in ESR1-mutant cell lines, providing another avenue for targeted therapies. The activation of the Wnt pathway also plays a crucial role in the promotion of the migration of select hotspot mutated cells.3
Tackling Acquired Immune Activation
In a second study, investigators sought to categorize ESR1 mutations through acquired basal-like features, which may be a key contributor to immunotherapy resistance.2 The analysis showed that ESR1 tumors have elevated expression of basal cytokeratins, a result not observed in wild-type tumors. This increased expression is associated with activation in pathways, including S100A8/S100A9-TLR4, representing potential blockade targets for future investigation.4
As the intricacies of ESR1 come into the spotlight, results from ongoing efforts to monitor and address resistance in patients with estrogen receptor–positive/HER2-negative breast cancer will be pivotal for personalized targeted treatment therapies. Efforts to address this are underway in the prevention of localized progression (TABLE).
For example, CDK4/6 inhibitors, such as palbociclib (Ibrance), have proven effective for acquired resistance in metastatic breast cancer. Results from PADA-1 (NCT03079011) have laid the groundwork for tracing ESR1 mutations in circulating tumor DNA over the course of hormonal therapy with an AI and palbociclib. When ESR1 mutations were detected, those who switched to fulvestrant in combination with palbociclib experienced a progression-free survival (PFS) that was nearly doubled compared with those who maintained treatment with the hormonal therapy following detection.6
Table
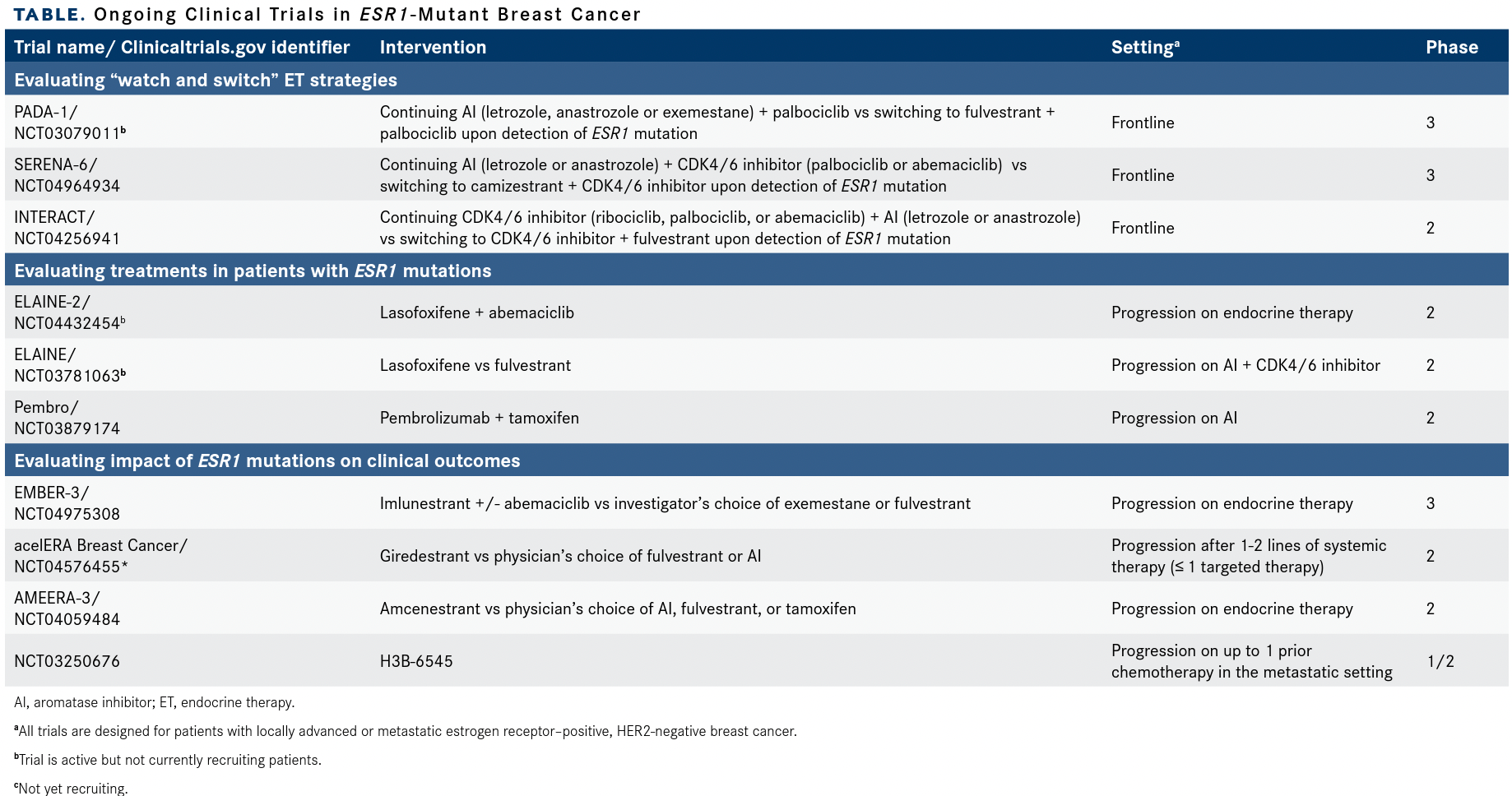
Rising mutations were detected prior to or concurrently with disease progression when assessed every 2 months using plasma analysis. Among a total of 1017 patients, 172 had detectable rising ESR1 mutations. These patients were randomly assigned to continue AI plus palbociclib (n = 84) or to crossover to fulvestrant plus palbociclib (n = 88). After a median follow-up of 26 months, median PFS was 11.9 months (95% CI, 9.1-13.6) for those who crossed over to fulvestrant vs 5.7 months (95% CI, 3.9-7.5) for those who did not (HR, 0.63; 95% CI, 0.45-0.88; P = .007).6
Novel strategies are also under investigation using this approach including using a novel oral selective estrogen receptor downregulator in place of an aromatase inhibitor in the phase 3 SERENA-6 trial (NCT04964934).
References
- Dustin D, Gu G, Fuqua SAW. ESR1 mutations in breast cancer. Cancer. 2019;125(21):3714-3728. doi:10.1002/cncr.32345
- Brett JO, Spring LM, Bardia A, Wander SA. ESR1 mutation as an emerging clinical biomarker in metastatic hormone receptor-positive breast cancer. Breast Cancer Res. 2021;23(1):85. doi:10.1186/s13058-021-01462-3
- Li Z, Wu Y, Yates ME, et al. Hotspot ESR1 mutations are multimodal and contextual modulators or breast cancer metastasis. Cancer Res. 2022;87(7):1321-1339. doi:10.1158/0008-5472. CAN-21-2576
- Li Z, McGinn O, Wu Y, et al. ESR1 mutant breast cancers show elevated basal cytokeratins and immune activation. Nat Commun. 2022;13(1):2011. doi:10.1038/s41467-022-29498-9
- Bahreini A, Li Z, Wang P, et al. Mutation site and context dependent effects of ESR1 mutation in genome-edited breast cancer cell models. Breast Cancer Res. 2017;19(1):60. doi:10.1186/s13058-017-0851-4
- Bidard FC, Hardy-Bessard AC, Bachelot T, et al. Fulvestrant-palbociclib vs continuing aromatase inhibitor-palbociclib upon detection of circulating ESR1 mutation in HR+ HER2– metastatic breast cancer patients: results of PADA-1, a UCBG-GINECO randomized phase 3 trial. Cancer Res. 2022;82(suppl 4):GS3-05. doi:10.1158/15387445.SABCS21-GS3-05