Article
F-627 Shows Strong, Durable Benefit in Chemotherapy-Induced Neutropenia in Breast Cancer
Author(s):
Efbemalenograstim alpha (F-627) has demonstrated strong and lasting benefit when used as a treatment for chemotherapy-induced neutropenia in patients with breast cancer, meeting the primary and secondary end points of a phase 3 study.
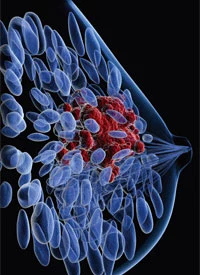
Efbemalenograstim alpha (F-627) has demonstrated strong and durable benefit when used as a treatment for chemotherapy-induced neutropenia in patients with breast cancer, meeting the primary and secondary end points of a phase 3 study (NCT03252431), according to recent announcement from Evive Biotech, the drug developer.1
“F-627 has now shown positive results in its pivotal phase 3 trial. We are excited that this trial has met its efficacy and safety end points as we believe it has the potential to positively impact cancer treatment,” William P. Daley, MD, Evive’s chief medical officer, commented in a recent press release. “F-627 has proven that it is at least as efficacious and safe as Neulasta, which is the current standard of care. This successful trial result reinforces F-627’s potential to be a strong first-line treatment, and an alternative for patients contraindicated or refractory to current treatment options.”
F-627 is a recombinant fusion protein that contains granulocyte colony–stimulating factor (G-CSF) at the amino terminal and human IgG2-Fc fragment at the carboxyl terminal. F-627 is expressed in Chinese Hamster Ovary cells, according to Evive, and it exists as a dimer with 2 molecules of rhG-CSF that are covalently connected through disulfide bonds forged between the Fc fragment of the molecule.
Additionally, F-627 induces the production of white blood cells, which play a key role in helping the immune system fight infection. Often, when patients are treated with chemotherapy, they experience a drop in white blood cells. F-627 was designed to boost those counts, and thus, strengthen immune system response.
The multicenter, single-dose, open-label, phase 3 trial evaluated the efficacy and safety of F-627 in women with stage I-III breast cancer receiving chemotherapy. The trial set out to enroll approximately 400 women with stage I-III invasive breast cancer who would receive neoadjuvant or adjuvant myelotoxic TC chemotherapy comprised of 75 mg/m2 of docetaxel and 600 mg/m2 of cyclophosphamide.2
Participants scheduled to undergo at least 4 21-day cycles of chemotherapy were included. Of note, patients were permitted to be scheduled for more than 4 cycles of chemotherapy treatment, but the study participation was limited to the patient’s first 4 cycles.
The primary goal of the trial was to examine the effectiveness of F-627 when administered at a single, fixed dose of 20 mg compared with pegfilgrastim (Neulasta), administered at the standard dose of 6 mg, in the first chemotherapy cycle. The primary end point of the trial is duration of grade 4 neutropenia, specifically the number of days in which the patient has had an absolute neutrophil count (ANC <0.5 x 10^9/L) observed in chemotherapy cycle 1. Secondary end points included duration in days of use of intravenous antibiotic and the duration in days of hospitalization, among others.
Twenty-four hours following the completion of chemotherapy in each cycle (day 2 of the cycle), patients received the 20-mg fixed dose prefilled syringe of F-627, given on day 2 of each of 4 chemotherapy cycles (arm 1) or the 6-mg fixed dose of pegfilgrastim, given on day 2 of each of 4 chemotherapy cycles (arm 2). Patients were randomized 1:1 to either of the 2 arms.
“F-627’s fusion protein structure presents a unique alternative as it reduces the possibility of allergic reactions caused by PEGylation used in pegfilgrastim,” Daley added. “It is also very encouraging to see that the treatment was well tolerated, with infection rates for those treated with F-627 lower than in the control arm of the trial, which was more pronounced in certain patient subgroups.”
Conducted under a Special Protocol Assessment in agreement with the FDA, the trial data will be submitted as part of a biologics license application (BLA) submission to the FDA and a market authorization application filing to the European Medicines Agency’s Committee for Medicinal Products for Human Use.
The global development program of F-627 is also comprised of successfully completed phase 3 trials that all met primary and secondary end points, according to Evive. The program includes 10 trials with over 1,200 participants.
Data with F-627 previously reported at the 2018 San Antonio Breast Cancer Symposium showed that the product significantly reduced the duration of grade 4 neutropenia in chemotherapy cycle 1 (P <.0001).3 The mean treatment difference was 2.8 days, with 1.1 days in the F-627 arm versus 3.9 days in the placebo arm. The administration of F-627 also led to a lower incidence and shorter duration of grade 2, 3, and 4 neutropenia.
The global study of 122 woman with stage II-IV breast cancer receiving myelotoxic chemotherapy also showed that treatment with the product also resulted in a significant reduction in the incidence of febrile neutropenia (P <.0016). Specifically, the incidence of this event in the investigational arm was 4.8% versus 28.2% in the placebo arm during cycle 1. Moreover, patients enrolled on the F-627 arm experienced lower rates of antibiotic and pain medication use.
With regard to safety, the product was determined to be safe and tolerable. No deaths or injection site reactions were reported, and less gastrointestinal toxicities were experienced by those in the experimental arm compared with those in the placebo arm. During cycle 1, the most common treatment-emergent adverse events (AEs) included leukopenia, anemia, thrombocytopenia, nausea, and alopecia. Across all treatment cycles, 17 serious AEs were reported in 15 participants; 15 of these events were febrile neutropenia.
“This moment is a key milestone for us as a business as we move toward submitting F-627’s BLA application to the FDA – one of the first Asian biologics companies to advance a novel biologic product from preclinical studies to BLA submission,” Jacky Liu, Evive’s CEO, stated in the press release. “As we begin the next stage of our journey, exploring commercialization partnerships to make this product available to patients worldwide, I would like to thank the Evive team, trial clinics, and doctors who have worked so tirelessly to develop this critical and potentially lifesaving treatment.”
References
- Evive Biotech meets primary and secondary endpoints in global phase III clinical trial for their novel chemotherapy-induced neutropenia treatment. News release. Evive Biotech. July 7, 2020. Accessed July 9, 2020. bit.ly/3gM43vQ.
- Neulasta-controlled trial of F-627 in women with breast cancer receiving myelotoxic chemotherapy. ClinicalTrials.gov. Updated February 5, 2020. Accessed July 9, 2020. https://clinicaltrials.gov/ct2/show/NCT03252431.
- Generon presented positive phase III results from a double-blind, placebo controlled-clinical trial of F-627 in women with breast cancer receiving myelotoxic chemotherapy. News release. Generon BioMed Holding Ltd. December 8, 2018. Accessed July 9, 2020. bwnews.pr/2ZVvWL2.









