Article
Innovations Are Poised to Lead MPN/MDS Treatment Landscape in a Positive Direction
Author(s):
Ahead of the 40th Annual Chemotherapy Foundation Symposium, Pinkal Desai, MD, addresses the evolving role of targeted therapies in MDS and how clinicians can characterize MDS risk.
Pinkal Desai, MD

A full day of programming on hematologic malignancies will kick off the 40th Annual Chemotherapy Foundation Symposium. Included in the lineup highlighting advances in multiple myeloma, leukemias, lymphomas, and other issues across malignancies, a portion of the afternoon programming will be dedicated to myeloproliferative neoplasms (MPNs) and myelodysplastic syndrome (MDS).
MPNs and MDS have traditionally been among the most difficult conditions for clinicians to address, often being accompanied by poor survival prognoses for patients, especially those in higher risk groups. However, there are several new tools and agents becoming available to clinicians to provide the best possible care for patients in this disease setting.
Ahead of CFS®, Pinkal Desai, MD, an assistant professor of medicine at Weill Cornell Medicine in New York, New York, joined OncLive® for an interview to discuss the session she will be moderating, “Myeloproliferative Neoplasms (MPNs)/Myelodysplastic Syndrome (MDS).” She addresses the evolving role of targeted therapies in MDS, how clinicians can characterize MDS risk, and other sessions she is anticipating at this year’s CFS®.
What are the primary updates that will be covered during the MDS session?
This year we want to highlight some of the upcoming data and new drug approvals in patients with MDS and MPN. There are 2 things that have happened this year that are different [in MDS].
One is the new World Health Organization 2022 classification that came out, which has some changes in how we classify MDS, particularly MDS with a SF3B1 mutation, which is a new category that will change some of the characterization of [patients with] MDS. They were previously considered clonal cytopenia of undetermined significance, and [these patients] did not have access to SF3B1-targeted therapies such as luspatercept. Now, a lot of them would be categorized as MDS SF3B1 mutations, expanding the role of luspatercept in these patients.
The other important factor in terms of risk stratification for MDS is that, for years, we knew the International Prognostic Scoring System [IPSS] or [revised] IPSS-R, which considers blood counts, cytogenetics, and chromosomal abnormalities in MDS, was important. [However], they were not telling the whole story of how a patient is predicted to behave. A lot of these so-called lower-risk patients were transforming sooner. Some others with intermediate risk were, maybe surprisingly, doing better.
Incorporation of molecular mutations in risk reduction was something we always thought was important. Now we have an IPSS-M, or IPSS molecular classification, which is available as a calculator for physicians to use online [Figure].1,2 This was based on a publication that was recently featured in the New England Journal of Medicine.2 We would have patients who were potentially lower risk in the past now moving to other risk categories like intermediate and beyond.
Figure. IPSS-M Risk Calculator for Myelodysplastic Syndrome1,2
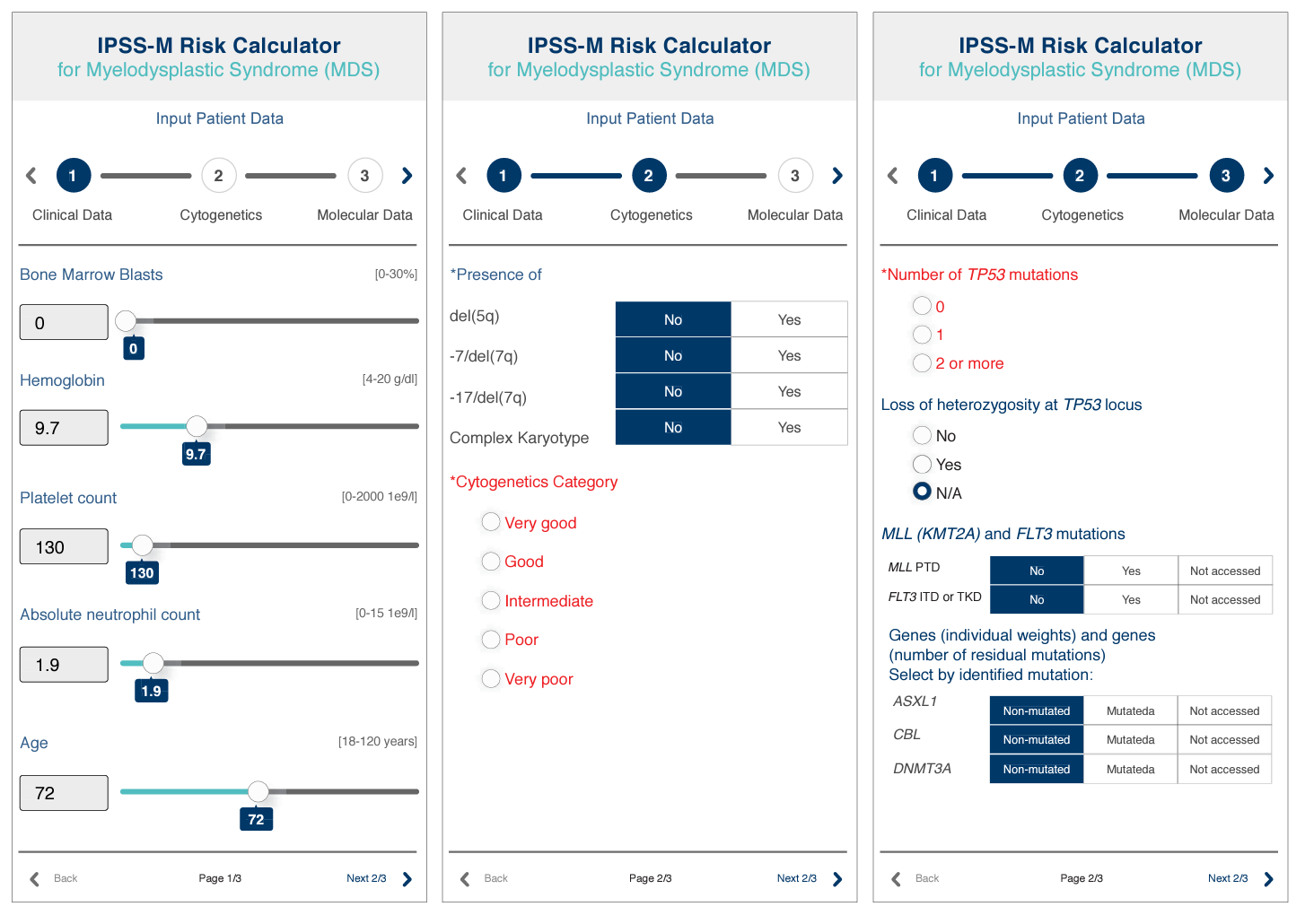
What do we do with that? We have had physicians [who] may have told patients how they would behave based on IPSS. How do you deal with this new information? Now the same patients might have a different risk, and how that would [possibly] lead to changes in treatment decisions is something that is important and will be covered at CFS®.
[Another example of] things that might change is transplant decisions based on what were considered lower-risk [patients] and [those who were] not to be transplanted. [That] could now change with the molecular classification. The molecular classification includes a lot of common mutations that physicians had information on, they just did not know how to incorporate it into the IPSS, which would now be game changing in understanding how patients will do.
What will also be interesting is how clinical trials adapt to this going forward. A lot of the clinical trials in the past were based solely on IPSS-R. With this new calculator, will clinical trials adapt to this? What happens to the trials that are still ongoing? There will be a lot of reclassification going forward.
In terms of treatment, we are covering [whether] there [is] a role for targeted therapies in MDS. MDS has been a difficult disease to treat in the myeloid space. We have had improvement in survival in acute myeloid leukemia [AML] and new drugs coming out for myeloproliferative disorders. [However], in MDS, all the phase 3 trials have been negative, but we have a lot of newer treatments coming forward.
On one hand, there are the immunotherapies in combination, such as CD47 antibodies in combination with hypomethylating agents [HMAs] or TIM3 inhibition with sabatolimab with HMA. On the other hand, you consider how AML has been doing that. Do we subclassify based on mutations? Are we going to target? If you have a patient with an IDH mutation, would you consider them as a separate entity and perhaps give a frontline IDH inhibitor? There are some data that were highlighted at [the 64th American Society of Hematology Annual Meeting and Exposition] last year, and we will be discussing some of those data.
[We will] also [cover] venetoclax [Venclexta]. It works, in theory, as more [of a] mutation-agnostic treatment. What its role is as a targeted agent in combination with HMA will be interesting to discuss. Will MDS become like AML, where we look at the mutations and think who should be treated with the targeted inhibitor vs [a] more global disease-targeting agent [such as] the immunotherapies? In theory, they could be treated either way.
We also have a session on disease-modifying agents in polycythemia vera [PV]. There has been a recent approval for ropeginterferon alfa-2b. It has been approved in PV for improving survival. In the past, patients with PV have been treated with phlebotomy or ruxolitinib. This is the first disease-modifying agent, but interferon use is controversial. There are a lot of institutions that do not use interferon. In the presence of these phase 3 randomized data, this will be an interesting discussion on how we change the standard of care for PV going forward, [as well as] what will happen to some of the other PV therapies that are undergoing clinical trials, [such as] hepcidin inhibitors.
Similarly in myelofibrosis, there have been several disease-modifying agents that have been used. [Additionally], there are several other clinical trials that are ongoing in myelofibrosis, including the use of BET inhibitors, which [are] showing good responses in patients with transfusion-dependent anemia or with anemia with myelofibrosis. There are several other agents all pushing toward the same category of patients, which is transfusion-dependent myelofibrosis, because that is a particularly difficult patient population to treat.
At the same time, a lot of the clinical trials are excluding patients with low platelets, which is also a clinical dilemma. If we do not have clinical trials that are allowing for these patients with low platelets, this becomes a challenge clinically, where anemia is important, and a lot of clinical trials are being developed in that category. What do we do about patients with low platelets and anemia? That will [also] be covered in this session.
What is the current role of targeted therapies in MDS? How do you see this evolving in the future?
First of all, it is uncommon to have these sorts of mutations that can be targeted. [Fewer] than 5% of patients with MDS will have an IDH mutation. But when you do find them, is it possible that targeted inhibitors do better than single-agent hypomethylating agents, or a combination of them?
There [are] some data that will be reviewed in our session suggesting promising outcomes of using IDH inhibitors in frontline patients with MDS, which would be game changing if it goes forward as the new standard. We are still awaiting more randomized phase 3 data in this regard. In the subset [of patients who] relapse after frontline hypomethylating agents, that is a very low-hanging fruit. These patients do not have a second-line option with MDS, and the role of IDH inhibitors in this setting is a slam dunk. [Findings are] suggesting good outcomes and transfusion independence in patients who have been treated with IDH inhibitors.
The other target mutation is TP53, and that has been a challenge. A lot of TP53-directed therapies have been used. We have had a recent phase 3 trial with APR-246 [NCT03745716], which was not successful in improving overall survival [OS].
CD47 antibodies or magrolimab is being used in this situation, although it is not a real targeted agent, because of some data that show there may be benefit in the subset of TP53 mutations. FLT3 inhibition is very rare in MDS. It is usually in AML that we FLT3 [inhibition useful].
When we talk about targeted inhibition, we are really talking about IDH and TP53 mutations. Could we have drugs that can specifically work against and target one of these mutations? Would MDS become how we think about AML right now, looking at mutations and then deciding therapies for these patients?
What is the role of disease-modifying agents in PV?
The current therapy for PV includes treatment with phlebotomy, hydroxyurea, or ruxolitinib, which are all approved in this space. [However], it was not clear whether any of these agents were improving OS. We have data, [which] will be discussed at CFS®, showing that ropeginterferon use in PV is associated with improved OS. This is as a game changer in patients with PV, because there were several institutions that were using interferon-based therapies for MPNs.
If you monitor these [groups of patients with MPNs], you will see that some patients are on interferon and others have never heard of it. Now that we have a clinical trial showing survival benefit, this will be an interesting discussion and would [potentially] change the of standard of care. What will physicians think of it in terms of adopting the use of interferon in PV?
What is the main takeaway you want your colleagues to come to following your session?
There is a lot of new drug development happening in patients with MDS and myeloproliferative diseases. With MPNs, you are focusing on survival. [There are] novel agents beyond JAK inhibition, particularly in transfusion-dependent myelofibrosis, and there are several upcoming new drugs and clinical trials.
We want to focus [on the fact] that there is growth in this space. There may be better combination therapies coming up front, including targeted inhibitors. There are also better prognostic classifications with MDS that are very different than what have been used so far. That would change the discussion physicians would have with their patients. These are absolutely the new standard, and we want to focus on this molecular classification of MDS that is now available as a calculator to practicing clinicians.
References
- IPSS-M risk calculator for myelodysplastic syndromes (MDS). MDS Foundation. Accessed November 3, 2022. mds-risk-model.com
- Bernard E, Tuechler H, Greenberg PL, et al. Molecular International Prognostic Scoring System for myelodysplastic syndromes. NEJM Evid. 2022;1(7). doi:10.1056/EVIDoa2200008