Publication
Article
Oncology Live®
A New Generation of Drugs Targeting PD-1/PD-L1 Takes Shape in Oncology
Author(s):
Over the past decade, immunotherapy has established itself as one of the pillars of cancer treatment, thanks in large part to the success of monoclonal antibodies that target the immune checkpoint protein PD-1 or its main ligand, PD-L1.
Over the past decade, immunotherapy has established itself as one of the pillars of cancer treatment, thanks in large part to the success of monoclonal antibodies (mAbs) that target the immune checkpoint protein PD-1 or its main ligand, PD-L1.1 The FDA has approved 6 anti–PD-1/PD-L1 immune checkpoint inhibitors (ICIs) covering 16 cancer indications as monotherapy or in combination with other drugs. ICIs also made history for having the first tissue-agnostic indications, with several agents approved across cancer types with microsatellite instability-high (MSI-H) or DNA mismatch repair–deficient (dMMR) biomarkers.2,3
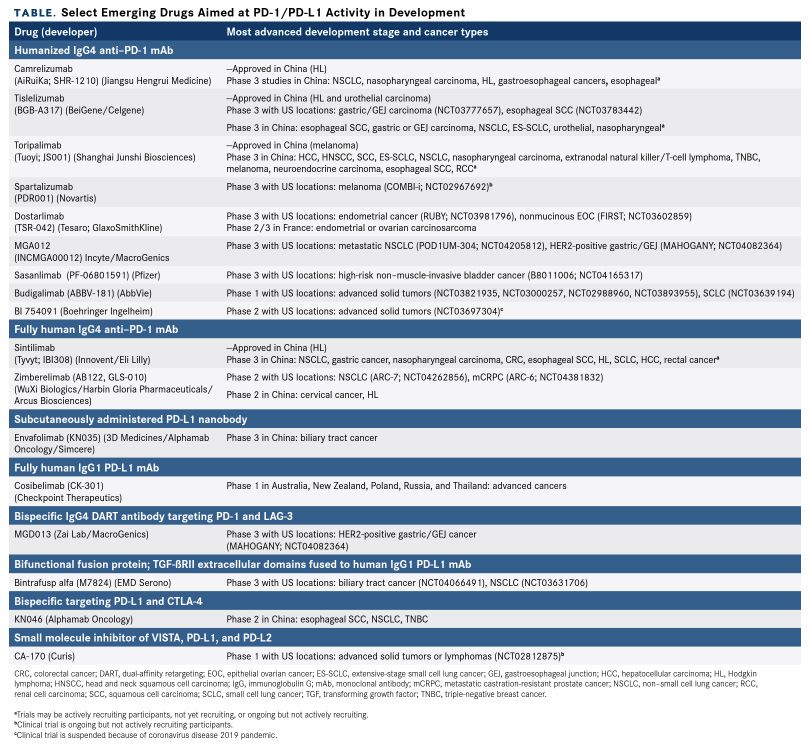
Now a new generation of ICIs targeting the PD-1/PD-L1 pathway is in the works, with numerous drug companies trying to develop their own offerings (Table). According to a recent analysis, nearly 3000 clinical trials testing PD-1/PD-L1 inhibitors were recruiting participants across most cancer types as of September 2019, with a total target enrollment of more than half a million patients.2
Biotechnology companies based in China are particularly active in the field. Chinese regulators have approved 4 PD-1 inhibitors developed domestically in addition to agents from international pharmaceutical firms,4-8 and several other novel therapies are in late-stage clinical testing.
In an increasingly crowded space, the focus is on novel strategies that might help a drug stand out from the crowd while also addressing limitations of ICI efficacy. Accordingly, 76% of ongoing clinical trials of PD-1/PD-L1 inhibitors involve combination therapy, predominantly with chemotherapy, tyrosine kinase inhibitors, and other types of ICIs.2 Investigators are also using new drug designs to combine different mechanisms into a single molecule. Bispecific antibodies and fusion proteins are demonstrating early promise across several tumor types.
Yet the dizzying pace of drug development has been curbed in recent months by the coronavirus disease 2019 pandemic. Regulatory agencies are providing assistance, and other government agencies have released guidance for investigators whose trials are affected. Nonetheless, these are challenging times, with patients reluctant to enroll in trials or unable to reach hospitals, in addition to laboratories being shut down and investigators retasked to serve on the front lines. Globally, companies have had to modify or even halt ongoing clinical trials, and the future is likely to be uncertain for some time.9,10
The Checkpoint in Action
The cancer immunologist George Klein wrote that “cancer derives from self-somatic cells, and therefore cancer immunity is a matter of breaking self-tolerance, which is a difficult proposition.” The discovery of the PDCD1 gene in the 1990s has brought the oncology community a long way toward achieving that challenging goal.11-13
PDCD1 encodes PD-1, a type I transmembrane receptor originally identified as being involved in the programmed cell death of immune cells. The receptor has subsequently been shown to play an important role in the checks and balances on the immune system that maintain self-tolerance to prevent collateral damage from the immune response, such as that seen in autoimmune diseases.11,13,14
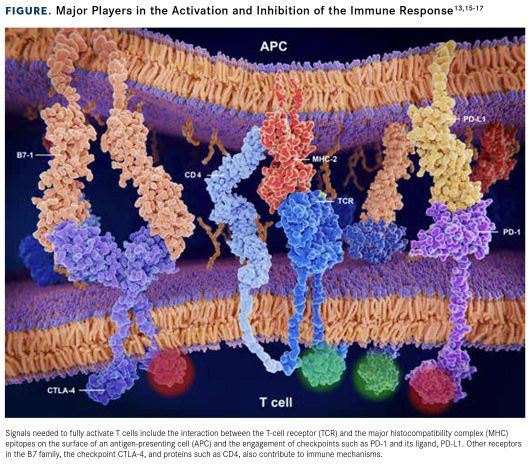
PD-1 is a member of the B7/CD28 family of receptors that share a common structure: an immunoglobulinlike extracellular domain, a transmembrane domain, and an intracellular domain containing the immunoreceptor tyrosine-based inhibitory and signaling motifs (ITIM and ITSM, respectively).13,15-17
ITIM and ITSM are phosphorylated when PD-1 is engaged by either of its ligands, PD-L1 or PD-L2, leading to recruitment of the SRC homology phosphatases SHP1 and SHP2, which transmit the signal into the cell. PD-1 is predominantly expressed on activated T cells, the major cytotoxic effectors of the adaptive immune response, and the signal it transmits helps to damp down the T-cellmediated immune response.13,15-17
Two separate signals are required to fully activate T cells that keep cytotoxic actvity in check. The first comes from the interaction between the T-cell receptor and major histocompatibility complex–presented antigen epitopes on the surface of an antigen-presenting cell (APC). The second comes from engagement of costimulatory receptor-ligand pairs on the T-cell and APC surfaces (Figure13,15-17). PD-1 belongs to a group of coinhibitory receptors that regulate T-cell activity via ligand binding, which can drive T cells into a state known as exhaustion, in which they are unable to proliferate or perform their effector functions.13,15-17
PD-L1 and PD-L2 are also transmembrane proteins that are identical in almost 40% of their amino acid sequence but differ in their affinity for PD-1 and the cell types and tissues in which they are expressed, with PD-L1 expression more widespread. They are characteristically constitutively expressed on the surface of APCs. However, their expression can also be induced on other cell types in response to inflammatory signals.13,15-17
Breaking Self-Tolerance
As Klein pointed out, tumors develop from the body’s own cells and should not provoke an immune response; however, many of the aberrant cellular processes that drive cancer development generate unusual proteins that can be recognized by the immune system as foreign antigens. Although this immune surveillance can eliminate cancer cells, selective pressure can ultimately cause them to evade the antitumor immune response through a variety of mechanisms. Indeed, immune evasion is now widely recognized as a hallmark of cancer.18,19
Exploitation of immune checkpoints like PD-1 is one of these mechanisms. PD-L1 is overexpressed on the surface of many different tumor types, including melanoma, lymphomas, and lung, breast, bladder, kidney, and brain tumors. This enables tumors to engage any T cells that infiltrate them and essentially switch them off.13,15-17
PD-L1 expression in tumors can be constitutive, as a by-product of oncogenic driver mechanisms, or induced by upregulated inflammatory signals produced by the tumor microenvironment. PD-L1 can also be expressed by myeloid cells in the tumor microenvironment, such as macrophages and dendritic cells.13
Antibody Development
The clinical success of mAbs targeting PD-1 and PD-L1 is an attractive lure, and drug development in this sphere continues at a robust pace. Numerous companies headquartered in the United States and Europe have entered the game, with their own PD-1 and PD-L1 mAbs in clinical development. But fierce competition is driving them to seek new ways to differentiate themselves.
Spartalizumab
One way to distinguish these agents is to pursue combination therapies that might expand the efficacy of PD-1/PD-L1 therapy, which is not effective in all patients. Notable in this respect is Novartis’ spartalizumab (PDR001), a humanized immunoglobulin (Ig) G4–based PD-1–targeted mAb.20 Early findings from the phase 3 COMBI-i trial (NCT02967692) evaluating melanoma treatment with spartalizumab, in combination with the BRAF inhibitor dabrafenib (Tafinlar) and the MEK inhibitor trametinib (Mekinist), continue to show promising efficacy, according to updated results from the 2020 American Society of Clinical Oncology (ASCO) Annual Meeting.21
Pooled data from 36 patients enrolled in run-in and biomarker cohorts demonstrated an investigator-assessed objective response rate (ORR) of 78%, including 44% with complete responses (CRs). Median duration of response had not been reached after a median follow-up of 24.3 months, but the 24-month rate was 53.4%. The median progression-free survival (PFS) was 22.7 months, and the median overall survival (OS) had not been reached.
Grade 3 and higher treatment-related adverse events (TRAEs), most commonly pyrexia, neutropenia, and increased lipase levels, occurred in 72% of patients, and 17% of patients experienced events that led to discontinuation of all 3 study drugs.21
COMB-i is continuing as a randomized study in which approximately 500 patients with previously untreated resectable metastatic BRAF V600–mutated melanoma will receive either the triplet therapy that includes spartalizumab or doublet therapy with the 2 targeted agents.
Dostarlimab
Tesaro, which GlaxoSmithKline acquired in 2019,22 has developed the humanized antiPD-1 IgG4 mAb dostarlimab (TSR-042). Several phase 3 clinical trials are ongoing, including in patients with endometrial cancer. Investigators presented results from cohorts of patients with endometrial cancer treated in the phase 1/2 GARNET trial (NCT02715284) at the 2019 Society of Gynecologic Oncology Annual Meeting on Women’s Cancer.
Participants (N = 110) received dostarlimab 500 mg every 3 weeks for the first 4 cycles and then 1000 mg every 6 weeks thereafter. Overall, the ORR was 27.7% and the disease control rate was 48.9%, with ongoing responses at data cutoff in most patients who exhibited a response. However, patients with MSI-H tumors had a particularly impressive ORR of 50% compared with 19.1% in patients with microsatellite-stable disease.23 In an updated interim analysis published in March 2020, the ORR was 43% among GARNET participants (N = 70) with dMMR disease and at least 6 months of follow-up at the data cutoff of July 8, 2019.24
Cosibelimab
Checkpoint Therapeutics is developing cosibelimab (CK-301), a fully human IgG1 mAb against PD-L1.13 Investigators presented positive interim data from a first-in-human study (NCT03212404) at the 2019 European Society for Molecular Oncology meeting. At the data cutoff in August 2019, 68 patients had at least 2 tumor assessments or had discontinued treatment, and the ORR across tumor types was 27.9%. The ORRs in cohorts of patients with cutaneous squamous cell carcinoma (CSCC; n = 14) and non–small cell lung cancer (NSCLC; n = 25) were 50% and 40%, with ongoing responses in 100% and 90% of responders, respectively.
Grade 3 or higher TRAEs occurred in 33.3% of patients. The most common any-grade TRAEs were rash, fatigue, hypothyroidism, anemia, elevated alanine aminotransferase levels, diarrhea, and infusion-related reaction.25 Checkpoint Therapeutics reported that based on positive feedback from the FDA, it intends to submit cosibelimab for approval as a CSCC treatment based on data from this trial.26
East Meets West
As Western markets become increasingly saturated with PD-1/PD-L1 inhibitors, pharmaceutical companies are seeking to expand into new areas, particularly in China and other Asian countries. Nivolumab (Opdivo), pembrolizumab (Keytruda), atezolizumab (Tecentriq), and durvalumab (Imfinzi) were recently approved by the Chinese regulatory agency, the National Medical Products Administration (NMPA). The approvals were for single indications (lung cancer), except pembrolizumab, which became the first to secure 2 approved indications in China (NSCLC and melanoma).5-8
With China’s status as the second-leading pharmaceutical market and foremost emerging market worldwide,27 an increasing trend toward development of PD-1/PD-L1 inhibitors has recently surfaced among Chinese biotechnology companies.2 Several drugs are in clinical trials, and the NMPA has approved 4 in the past 18 months: camrelizumab (AiRuiKa), sintilimab (Tyvyt), toripalimab (Tuoyi), and, most recently, tislelizumab (BGB-A317).2,4
All these drugs are approved in China for Hodgkin lymphoma treatment. Additionally, toripalimab is approved for melanoma,28 and tislelizumab is indicated in metastatic urothelial carcinoma.29 Phase 3 trials in numerous indications are ongoing.
BeiGene reported results at ASCO 2020 from an ongoing phase 3 trial of tislelizumab in combination with chemotherapy for the firstline treatment of advanced squamous NSCLC (NCT03594747); the study is being conducted at multiple sites in China. The addition of tislelizumab to paclitaxel and carboplatin (arm A) or to nab-paclitaxel (Abraxane) and carboplatin (arm B) improved PFS more than paclitaxel plus carboplatin. The median PFS in the 3 arms, respectively, was 7.6 months (HR, 0.52; P = .0001), 7.6 months (HR, 0.48; P <.0001), and 5.5 months. Serious TRAEs in the 3 arms were reported in 36.7%, 38.1%, and 24.8% of patients, respectively.30
Among the drugs in clinical development is envafolimab (KN035), a single-domain antibody (nanobody) against PD-L1 and the first PD-1/ PD-L1 inhibitor to be developed as a subcutaneous formulation.16 Envafolimab showed promising safety and preliminary antitumor efficacy in patients with advanced solid tumors in phase 1 results presented at ASCO 2019.31 In a phase 2 study (NCT03667170), envafolimab demonstrated confirmed ORRs of 30% among 50 patients with MSI-H/dMMR advanced cancers, including colorectal and gastric cancers, according to interim findings reported at ASCO 2020. The ORR was 54.2% in the cohort of patients with colorectal cancer who had undergone prior chemotherapy.32
During a session titled “East Meets West: Chinese Pharma Explores Western Markets” held at the American Association for Cancer Research meeting in 2019, Richard Pazdur, MD, the director of the FDA’s Oncology Center of Excellence, urged Chinese companies to bring their PD-1/PD-L1 drugs to the US market in an effort to reduce prices.33
US and Chinese drug developers have already forged numerous collaborations. BeiGene has entered into an agreement with Celgene to develop and commercialize tislelizumab for the treatment of solid tumors in all non-Asian countries and Japan, with BeiGene retaining exclusive rights in Asian countries other than Japan.34 Innovent Biologics and Eli Lilly reached a similar partnership for sintilimab commercialization.33 Additionally, California-headquartered Arcus Biosciences licensed the PD-1 mAb zimberelimab (AB122, GLS-010) from WuXi Biologics and its partner Harbin Gloria Pharmaceuticals.35,36
In With the New
Companies are also seeking to improve efficacy by pursuing combination therapy, rather than monotherapy, right out of the gate. Besides chemotherapy and radiation therapy, the most popular additions to PD-1/PD-L1 inhibitors include VEGF inhibitors, other ICIs, and costimulatory receptor agonists.2
These strategies seek to overcome potential mechanisms of resistance to PD-1/PD-L1 inhibition and capitalize on synergistic antitumor activity. In addition to its role in angiogenesis, VEGF is thought to function in immune suppression.37 A host of other coinhibitory receptors exist, including CTLA-4 and LAG-3,38 against which mAbs are available. Meanwhile, agonists of costimulatory receptors, such as OX40, and their ligands have also been developed to boost T-cell activation.39
Manufacturers are also employing novel drug designs to capture combined mechanisms of action in a single molecule. Several bispecific antibodies and fusion proteins are in clinical development. These include bintrafusp alfa (M7824), a bifunctional fusion protein comprising tumor growth factor (TGF)-ßRII extracellular domains linked to a PD-L1 mAb, that EMD Serono is developing.40
Cancer cells frequently express the cytokine ligand TGF-ß, which exerts immunosuppressive effects that can hamper the efficacy of PD-1/ PD-L1 inhibitors.41 EMD Serono has advanced bintrafusp alfa into a head-to-head trial against pembrolizumab in the first-line treatment of PD-L1–positive NSCLC (NCT03631706).
Meanwhile, results from several expansion cohorts of an ongoing phase 1 trial of bintrafusp alfa (NCT02517398) have been reported at various recent conferences. Among 33 patients with heavily pretreated triple-negative breast cancer, 1 confirmed CR and 2 partial responses (PRs) were reported, and the median PFS and OS were 1.3 months and 7.8 months, respectively. Grade 3 TRAEs included anemia, asthenia, decreased appetite, rash, hypophysitis, and increased transaminases, with 1 death related to treatment.42
Among 25 patients in the cervical cancer expansion cohort, 6 confirmed responses (ORR, 24%) were reported, with 5 ongoing at data cutoff, as was an additional delayed PR. Grade 3 TRAEs occurred in 24% of patients, and 1 patient had grade 4 treatment-related hypokalemia. No deaths related to bintrafusp alfa treatment occurred.43
Finally, in 80 patients with chemotherapy-pretreated but immunotherapy-naïve advanced NSCLC, bintrafusp alfa therapy was associated with an ORR of 21.3% across the entire population, who had been treated with either 500 mg or 1200 mg every 2 weeks. Among patients who received the 1200-mg dose, the ORR was 36% (10 of 27 patients) in those with PD-L1–positive disease (≥1% expression) and 85.7% (6 of 7 patients) in those with high PD-L1 expression (on ≥80% of tumor cells). TRAEs occurred in 69% of patients, with grade 3 or higher TRAEs in 29%, and no treatment-related deaths were observed.44 In 2-year follow-up data reported at ASCO 2020, 18- and 24-month PFS and OS rates among those who received the 1200-mg dose were 18.4% and 11.0%, and 49.7% and 39.7%, respectively. At that dosage, the median OS was 21.7 months in those with PD-L1–positive tumors.45
Biotechnology companies are also pursuing small molecule inhibitors of PD-1/PD-L1, facilitated by publication of the crystal structure of the receptor-ligand complex in 2015.46 Small molecule inhibitors could overcome many of the limitations of mAbs, such as their poor penetration of solid tumors, inconvenient intravenous administration, daunting toxicity profiles, and costly production.16,17
Most of these drugs are still in preclinical development. However, Curis and its partner Aurigene are testing CA-170, a small molecule inhibitor of PD-L1, PD-L2, and the VISTA immune checkpoint protein, in a phase 1 trial in advanced solid tumors (NCT02812875), although questions about its ability to bind to PD-L1 have recently arisen.47




























%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
