Publication
Article
Oncology Live®
A View From the Frontlines: How a Hospital System Coped With a COVID-19 Peak
Early in the pandemic, the Montefiore hospital leadership had the forethought and insight to create a reliable and robust outcomes data collection system on all patients with a diagnosis of COVID-19 being seen and treated within the system.
Vikas Mehta, MD, MPH, FACS, is a surgical oncologist at Montefiore Health System, and an associate professor of Otorhinolaryngology–Head and Neck Surgery at Albert Einstein College of Medicine in Bronx, NY.

In early March 2020, the news reported a “superspreading” event in the town of New Rochelle, New York, a suburb with a Montefiore hospital that borders the Bronx where the flagship Montefiore hospitals are located. Soon after, in what seemed to be only possible in a dystopian fictional narrative, the National Guard arrived to assist with quarantining the area. We were told the source patient had no known sick contacts and no history of travel to a “hot zone.” I discussed with a colleague the catastrophic implications and potential for widespread disease dissemination. Within several days, the governor ordered, “New York State was on PAUSE,” which outlined the official closing plan, and Montefiore Health System was bracing for an onslaught of coronavirus disease 2019 (COVID-19) cases.
Early in the pandemic, it was clear that the risk posed to vulnerable populations exceeded that of the rest of the population. Patients with cancer would ostensibly be at higher risk of developing and succumbing to COVID-19 due to immunosuppression, increased coexisting medical conditions, and, in cases of lung malignancy, underlying pulmonary compromise. Patients with hematologic cancers, or those receiving active chemotherapy or immunotherapy, also might be particularly susceptible due to increased immunosuppression and/or dysfunction.
Leadership at Montefiore Einstein Center for Cancer Care rapidly instituted measures to protect our patients while simultaneously attempting to avoid disruption to patients receiving ongoing cancer treatment. What complicated things further was that the virus causing COVID-19 infections had been circulating in our community for weeks. The effects were seen in our oncology clinics and COVID-19 wards.
As New York emerged as the pandemic epicenter in the United States, we felt it was our duty to report on the case-fatality rate within our oncology population to inform other health care systems, patients with cancer, and the public about oncologic patients’ particular vulnerability to this COVID-19.
A group of physicians from medical, radiation, and surgical oncology quickly banded together to gather data on COVID-19–infected oncology patients. We greatly benefited from existing databases that allowed us to rapidly identify and extract baseline data from our hospital system, which extends from New York City to upstate New York.
Early in the pandemic, the Montefiore hospital leadership had the forethought and insight to create a reliable and robust outcomes data collection system on all patients with a diagnosis of COVID-19 being seen and treated within the system. We were able to marry this data set with an existing database created to identify patients with cancer, and track treatment volumes and timelines of care in real time.1
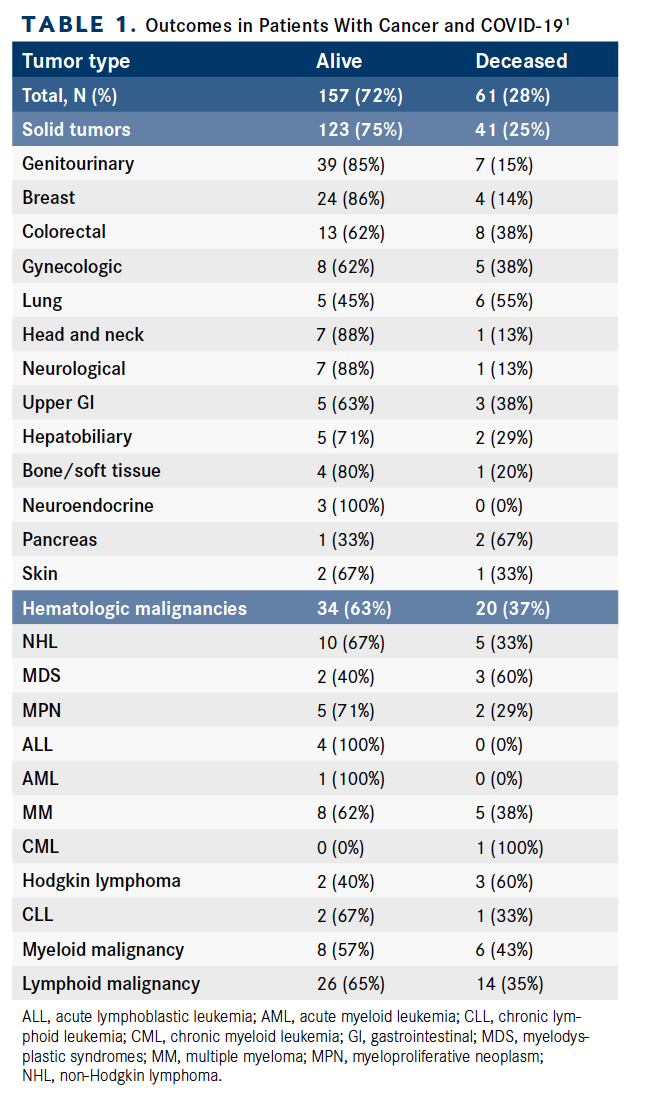
A total of 218 patients with cancer and COVID-19 infection from March 18 to April 8, 2020, were identified. The database included 164 (75%) patients with solid tumors and 54 (25%) with hematologic malignancies (Table 1).1 Sixty-one (28%) patients died from COVID-19 infections. The mortality rate was 25% of all patients with solid tumors. The highest rates of death occurred in patients with lung cancers (55%); gastrointestinal cancers, including colorectal (38%), pancreas (67%), and upper GI (38%); and gynecologic malignancies (38%). Genitourinary (15%) and breast cancers (14%) were associated with relatively lower mortality with COVID-19 infection. Hematologic malignancies were associated with higher case fatality rates (37%). Older age and comorbidities, such as concomitant heart disease—including hypertension, coronary artery disease, and chronic heart failure—and chronic lung disease, increased the risk of dying from COVID-19 in patients with cancer.
Interestingly, active disease (< 1 year) and advanced metastatic disease showed a trend for increased mortality, but the association did not achieve statistical significance (P = .09 and P = .06, respectively). Active chemotherapy and radiation therapy treatment were not associated with increased case fatality.
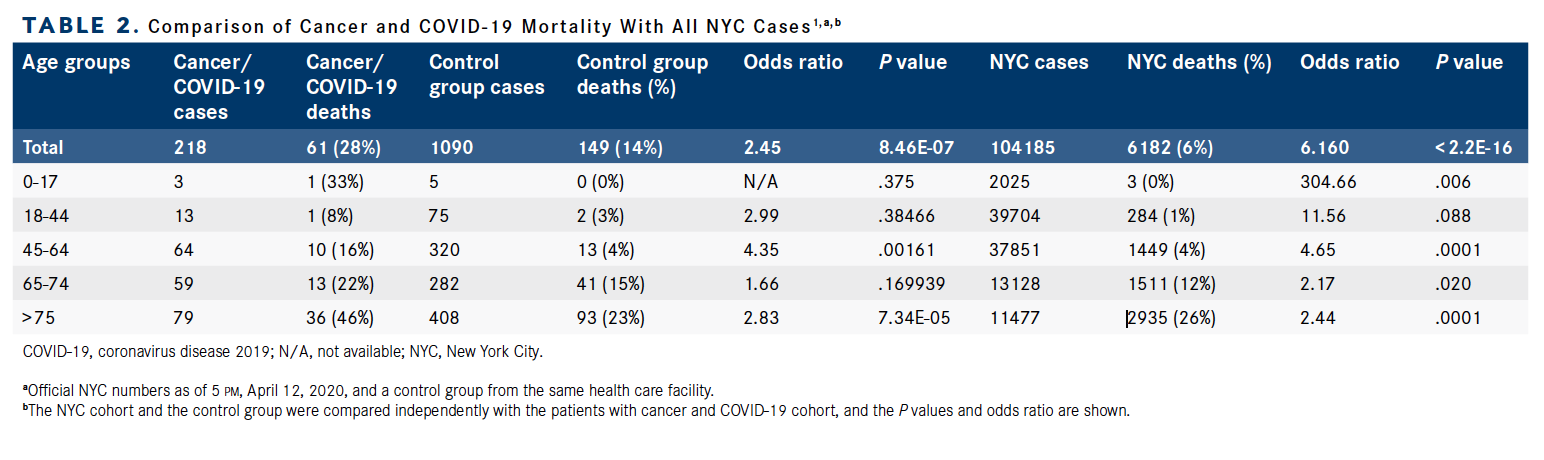
An age and sex-matched cohort of 1090 patients at a 5:1 ratio of patients without cancer to patients with cancer and COVID-19 from the same time period and from the same hospital system also was obtained after propensity matching. This was used as a control to estimate the increased risk posed to our cancer population.
We observed case fatality rates that were elevated in all age cohorts in patients with cancer and achieved statistical significance in the age groups 45 to 64 (OR, 4.35) and in patients older than 75 years (OR, 2.83). We also compared our case-fatality rates with a larger data set from the greater New York City region, and in all age cohorts, patients with cancer demonstrated a striking increase in case-fatality rates (Table 2).1
A detailed analysis of patients who died (N = 61) demonstrated that many were either nursing home or shelter (n = 22) residents, and/or admitted as an inpatient or came to the emergency room within the 30 days prior to their COVID-19 positive test (n = 21). Altogether, 37 patients (61%) in the deceased cohort were exposed to the health care environment at the outset of the COVID-19 epidemic, thus emphasizing the need for early social-distancing efforts, resources for more outpatient-based care and telemedicine, testing of asymptomatic high-risk patients, and institution of strict infection control measures for our most vulnerable patients. By acting immediately upon our findings, we ensured that the appropriate and best care possible could be delivered to our patients.1
Overall, our data suggested a significant risk posed to patients with cancer infected with COVID-19 with a measurable increase in mortality. The highest susceptibility appeared to be in hematologic or lung malignancies, suggesting that proactive strategies to reduce likelihood of infection and improve early identification of COVID-19 positivity are warranted in the population of patients with cancer.
In coming together to report on a large COVID-19–positive cancer cohort in the US epicenter, we were able to quickly translate our findings to clinicians and hospital professionals across the country. We also provided guidance to diminish the rate and consequences of this evolving infection in the vulnerable oncology population.
Our hope is that by reporting quickly on these data, lives of people with cancer can be spared. Our findings also inform cancer physicians on who could and should still be getting cancer treatment if precautions to separate people with cancer from others with COVID-19 infections are strictly followed.
Reference
Mehta V, Goel S, Kabarriti R, et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020;10(7):935-941. doi:10.1158/2159-8290.CD-20-0516
























%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
