- Vol. 22/No. 08
- Volume 22
- Issue 08
Clinical Progress Creates Need for Decision-Support Tools

The current endorsement of 3 COVID-19 vaccines in the United States, with several additional products pending FDA review, in less than 1 year from the identification of the structure of the COVID-19 virus is simply remarkable.
The history of vaccine development highlights the remarkable achievement associated with the establishment of several unquestionably safe and highly effective coronavirus disease 2019 (COVID-19) vaccines.1 In an analysis of more than 600 clinical trials, investigators found that the probability was only 10% for vaccines moving from phase 2 studies to FDA licensure within 10 years.1 Further, the average time for this approval to occur was 4.4 years. So the current endorsement of 3 COVID-19 vaccines in the United States (although the approvals are not formally complete), with several additional products pending FDA review, in less than 1 year from the identification of the structure of the COVID-19 virus is simply remarkable.
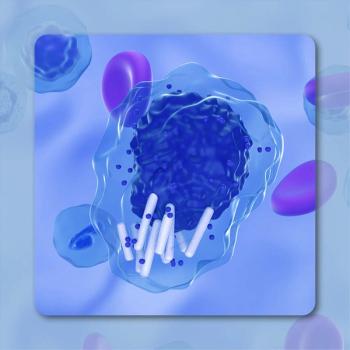
This accomplishment underscores the evolving successes associated with converting our understanding of basic molecular biology into major advances in human health and also characterizes the situation in anticancer therapeutics; progress in laboratory research (foundational and translational) is rapidly being transformed into meaningful benefits in the clinic.
Consider, for example, developments in a single, relatively common molecular abnormality in non–small cell lung cancer, the KRAS G12C mutation.2 In Western populations, KRAS mutations have been identified in as many as one-third of individuals with lung adenocarcinomas, with no currently available antineoplastic agent that effectively targets this critically relevant driver abnormality.2
Basic research efforts have provided a detailed understanding of the role of KRAS mutations in tumor progression and the critical opportunity that exists to impact disease progression. KRAS mutations are particularly observed in individuals with a current or past smoking history and are associated with both chemotherapy resistance and poorer clinical outcomes.2
The majority of KRAS mutations (80%) are found at codon 12, with several specific abnormalities being identified. The most common mutation (G12C) accounts for 40% to 50% of KRAS observed in lung adenocarcinomas, which have been shown to be associated with cisplatin resistance.2 In addition, the presence of a KRAS mutation has been associated with a high degree of resistance to EGFR inhibitors.2
However, promising early results have been reported with several antineoplastic agents that appear to effectively target KRAS G12 mutations, administered both as single agents and in combination strategies. It is reasonable to anticipate that one drug—and likely more drugs—in this category will be approved relatively soon for the noninvestigative treatment of lung cancer.2
Putting Knowledge Into Action
Although there is genuine excitement among physicians caring for patients with lung cancer about the prospects for these new therapies, one must painfully acknowledge the critical issue of the minimal decision-support approaches available for those adding these drugs to the portfolio of chemotherapy, targeted, and immunotherapeutic antineoplastic agents used to treat this disease entity. Clinicians will also be required to consider issues of single-agent vs combination therapy, optimal sequencing of management strategies, the increasing use of molecular diagnostics, and individual insurance company–mandated pathways.
One only need consider the current state of the use of PARP inhibitors in the treatment of patients with epithelial ovarian cancer to appreciate the rapidly evolving complexity of choices associated with expanding therapeutic options. There are now 3 FDA-approved PARP inhibitors for both active therapy and maintenance, with different single- agent and combination approaches to be considered in multiple settings.3 Further, clinicians must now include a decision to either employ or not utilize molecular testing, either for single gene defects or more complex molecular signatures for homologous recombination deficiency, in their management decisions for individual patients.
Finally, added to this list of clinical considerations are evolving evidence-based pathways that are not directly related to specific anti-neoplastic therapeutics but rather to supportive efforts in unique clinical settings, such as the requirement for venous thromboembolism prophylaxis.4
This steady increase in available therapeutic options in multiple cancers types and clinical settings that need to be considered and subsequently discussed with patients is occurring during an era when many physicians are simply unable to spend sufficient time to permit such deliberations. A recent report involving 155,000 physicians in 417 health systems in the United States that included data from 100 million patient encounters revealed that clinicians spent a large percentage of their time directly interacting with the electronic medical record (chart review, documentation, ordering) rather than in direct conversation and discussion with the patient.5
How do these developments affect optimal patient care in the oncology arena? To be clear, the goal of all oncology providers is to provide the highest-possible level of care.
However, consider the following: Despite the fact that obtaining germline genetic testing on all women diagnosed with epithelial ovarian cancer has been strongly recommended for a number of years by multiple national organizations, only 34.3% of such patients had undergone such testing, according to results of a recent analysis of population-based data in California and Georgia.6 This is for molecular testing, principally BRCA mutations, that is universally recognized to be of benefit not only for the individual patient but also for family members.
Of course, the conclusion here is not that oncologists are unwilling to obtain such testing, but rather that they are simply overwhelmed with the magnitude of the rapidly increasing requirements associated with the provision of optimal care. And, although there is certainly no single solution to this complex issue, one critical component of the answer must be the development of relatively simple, cost-effective, and highly robust decision-support tools.
References
- MacPherson A, Hutchinson N, Schneider O, et al. Probability of success and timelines for the develop-ment of vaccines for emerging and reemerged viral infectious diseases. Ann Intern Med. 2021;174(3):326-334. doi:10.7326/M20-5350
- Burns TF, Borghaei H, Ramalingam SS, Mok TS, Peters S. Targeting KRAS-mutant non-small-cell lung cancer: one mutation at a time, with a focus on KRAS G12C mutations. J Clin Oncol. 2021;38(35):4208-4218. doi:10.1200/JCO.20.00744
- Chan JK, Liang SY, Kapp DS, et al. Selecting new upfront regimens for advanced ovarian cancer with biomarker guidance. Gynecol Oncol. 2020;159(3):604-606. doi:10.1016/j.ygyno.2020.09.017
- Key NS, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2020;38(5):496-520. doi:10.1200/JCO.19.01461
- Overhage JM, McCallie D Jr. Physician time spent using the electronic health record during outpatient encounters: a descriptive study. Ann Intern Med. 2020;172(3):169-174. doi:10.7326/M18-3684
- Kurian AW, Ward KC, Abrahamse P, et al. Time trends in receipt of germline testing and results for women diagnosed with breast cancer or ovarian cancer, 2012-2019. J Clin Oncol. Published online February 9, 2021. doi:10.1200/JCO.20.02785
Articles in this issue
almost 5 years ago
New Approaches Seek to Meet the Challenge of Graft-Vs-Host Diseasealmost 5 years ago
Landscape for Unresectable HCC Comes Into Sharper Focusalmost 5 years ago
Phase 1/2 Studies Set the Stage for Targeted Combos in B-Cell Lymphomasalmost 5 years ago
RET Inhibition Holds Tumor-Agnostic Potentialalmost 5 years ago
Apalutamide Maintains OS Benefit in Castration-Sensitive Prostate Canceralmost 5 years ago
A Desire to Be a Healer Drives Breast Cancer Expert Forwardalmost 5 years ago
Pandemic Intensifies the Struggle With Burnout in Cancer Fieldalmost 5 years ago
Umbralisib Expands the Treatment Landscape for Non-Hodgkin Lymphomas



































