Publication
Article
Oncology Live®
PI3K Inhibitors and Oral Taxanes for Metastatic Breast Cancer: Where Do They Fit In?
Author(s):
A panel of experts in breast cancer discuss the emergence of alpelisib, review data from the BYLieve trial, discuss the role of everolimus, and review the emergence of oral taxanes.
Hope S. Rugo, MD, FASCO

Treatment options for metastatic breast cancer continue to expand, and new drug classes and new formulations of tried-and-true agents have emerged, providing clinicians with more opportunities to individualize treatments and improve outcomes. One major recent development was the May 24, 2019, approval of the first PI3K inhibitor, alpelisib (Piqray), for patients with PI3K mutations of PIK3CA, which have been associated with a poor prognosis and treatment resistance.1-3 However, although agents such as alpelisib are expanding treatment options for certain patient subsets, chemotherapy remains a mainstay of treatment for many patients across the metastatic breast cancer spectrum. Currently, only intravenous (IV) options are available, but traveling to infusion centers can be burdensome for patients and may pose health risks, particularly while the world is still grappling with the coronavirus disease 2019 (COVID-19) pandemic. An expected advance is the imminent approval of 1 or more oral taxanes, which have the potential to mitigate these challenges and risks but may have some drawbacks of their own.
During an OncLive Peer Exchange®, a panel of experts in breast cancer discussed the emergence of alpelisib and provided insights into the timing of testing patients for PIK3CA mutations. They reviewed data from the phase 3 SOLAR-1 trial (NCT02437318), which led to alpelisib’s approval, as well as data from the phase 2 BYLieve trial (NCT03056755), which recently provided reassurance regarding the use of this treatment in patients previously treated with CDK4/6 inhibitors.2,3 They also examined strategies for mitigating alpelisib’s adverse effects (AEs) and discussed the role of everolimus (Afinitor) in a world post alpelisib. Finally, the panelists reviewed the emergence of oral taxanes, focusing on data for oral paclitaxel and encequidar (formerly known as Oraxol), and discussed the potential advantages and disadvantages of this approach.
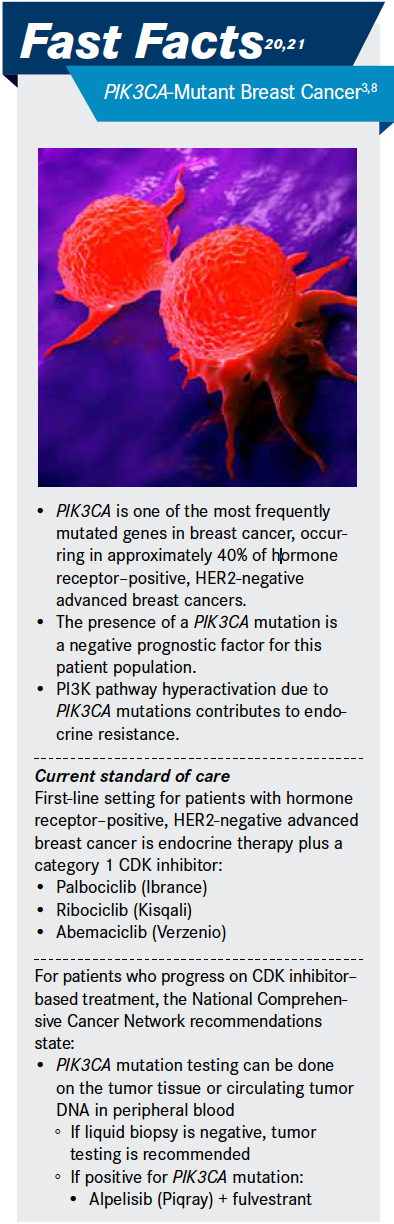
PI3K Inhibitors
PIK3CA mutations occur in approximately 40% of patients with hormone receptor– positive, HER2-negative advanced breast cancer.2,3 Because this is an actionable mutation, the panelists discussed the importance of assessing for it. “The first-line setting, often while using a CDK4/6 inhibitor, is a nice opportunity to start your molecular testing for PI3K status, knowing then that you may have an opportunity in later lines of therapy to use a PI3K inhibitor,” Tiffany A. Traina, MD, said.
Timing of PIK3CA mutation testing has not been clearly defined; however, the panelists agreed that they typically test patients when they are starting to fail first-line treatment, including CDK4/6 inhibitors. “We like to be organized and thinking ahead, but testing while somebody is responding to their current treatment might not be the best time to do it,” Claudine J. Isaacs, MD, said. Moderator Hope S. Rugo, MD, FASCO, concurred, saying,“I usually test when they’re starting to look like they might be progressing sometime in the near future.”
From a payer perspective, John Fox, MD, MHA, noted that the advent of molecular diagnostics has increased the probability that patients will receive the therapy that is most appropriate for their cancer type. However, he said confusion exists regarding coverage of the tests. “If you’re looking for a single gene mutation like a PIK3CA mutation, those tests are covered,” he said. “Typically when you get into these very costly nextgeneration sequencing tests, for example, if you have to do a liquid biopsy because you don’t have tissue, those tests require prior authorization to determine whether they’re medically appropriate.”
Patients found to have a PIK3CA mutation are candidates for alpelisib, which was approved in combination with fulvestrant (Faslodex) for postmenopausal women, and men, with hormone receptor–positive, HER2-negative, PIK3CA-mutant, advanced or metastatic breast cancer detected by an FDA-approved test following progression on or after an endocrine-based regimen.1
SOLAR-1 Trial
SOLAR-1 randomly assigned 572 patients, including 341 with PIK3CA mutations, 1:1 to oral alpelisib 300 mg daily plus fulvestrant 500 mg given as an intramuscular injection on days 1 and 15 of cycle 1 and on day 1 of 28 subsequent cycles or to equivalent oral placebo plus fulvestrant.2 The primary end point was investigator-assessed progression-free survival (PFS), and secondary end points included overall response rate and safety.
“There was improvement in PFS that was clinically meaningful, almost a 6-month improvement,” Priyanka Sharma, MD, said. At a median follow-up of 20 months, the alpelisib–fulvestrant group had a PFS of 11.0 months versus 5.7 months in the placebo group (HR for progression or death, 0.65; 95% CI, 0.50-0.85; P < .001). In contrast, the HR in the cohort without PIK3CA-mutant cancer was 0.85 (95% CI, 0.58-1.25; posterior probability of HR < 1.00, 79.4%).2
The most common alpelisib-related AEs included hyperglycemia, rash, and diarrhea. Grade 3 or 4 hyperglycemia occurred in 36.6% of alpelisib-treated patients and led to treatment discontinuation in 6.3% of patients.2 Because hyperglycemia is an on-target effect of alpelisib, potentially inextricably linked with α-specific PI3K inhibition, the panelists discussed the importance of managing this toxicity.
“We check baseline hemoglobin A1C [glycated hemoglobin] and talk about having a low-carb diet and finger-stick glucose monitoring,” Traina said. In patients showing elevation in their glycated hemoglobin levels, Isaacs said, she follows an algorithm to guide metformin dosing if treatment with metformin is not sufficient.
Rugo said she involves an endocrinologist because many newer hyperglycemia treatments may be useful in this setting. She also discussed the results of a recent presentation she gave at the European Society of Medical Oncology Congress 2019 that examined the course of AEs of special interest in SOLAR-1.4 “What we saw is that if you’re going to be hyperglycemic, you usually peak in the first 15 days,” she said. She said the same was true with rash, which is why she and her colleagues have started to encourage patients to use preventive, nonsedating antihistamines. “I think this is something like the steroid mouthwash that we used for everolimus stomatitis—we can really minimize that toxicity [of rash with alpelisib],” she said.
Given alpelisib’s availability, the panelists examined what role everolimus may play in treating patients with hormone receptor–positive, HER2-negative, PIK3CA-mutant advanced breast cancer. Everolimus became a standard treatment in combination with the steroidal aromatase inhibitor (AI) exemestane for patients with hormone receptor–positive, HER2-negative metastatic breast cancer resistant to prior nonsteroidal AI therapy after it received FDA approval in 2012 based on results of the BOLERO-2 trial (NCT00863655).5,6
Traina said everolimus still has a place but that it has moved down the line of potential options for endocrine therapy partnered with exemestane. “Sometimes in someone who’s had a small level of progression but needs a change of therapy, has sequenced through all our other available endocrine therapies, and perhaps is PIK3CA wild-type, I would see that as an option with the steroid rinse to make the mucositis more manageable, if you will, as an alternative to moving on to chemotherapy,” she said. The other panelists concurred and suggested it could also be a good option for patients who have difficulty with alpelisib’s AEs. “For patients who have a PIK3CA mutation and cannot tolerate alpelisib because of diarrhea, or for a small proportion who develop significant rash, this is a useful drug,” Sharma said. She noted, however, that it would not be appropriate for those who experienced pneumonitis while on alpelisib because they would be at high risk of having this same AE with everolimus.
One of the unknowns with alpelisib has been this agent’s efficacy in combination with fulvestrant in patients who have received contemporary first-line endocrine therapy plus targeted therapy, including a CDK4/6 inhibitor paired with AI or fulvestrant, regimens that currently have a National Comprehensive Cancer Network category 1 recommendation in this setting.7 Because of SOLAR-1’s timing, only 20 patients had received a prior CDK4/6 inhibitor. To better inform decision-making in such patients, investigators conducted the BYLieve trial.3 At the time of this Peer Exchange, no data were available for this trial; however, data regarding the cohort of patients who received a CDK4/6 inhibitor plus AI therapy immediately before second-line treatment with alpelisib plus fulvestrant have since been presented at the American Society of Clinical Oncology 2020 Virtual Scientific Program.3
BYLieve Trial
BYLieve is an ongoing, open-label, phase 2 trial that plans to enroll 340 patients across 3 cohorts: immediate prior CDK4/6 inhibitor plus AI therapy (enrollment complete), immediate prior CDK4/6 inhibitor plus fulvestrant (enrollment complete), and immediate prior systemic chemotherapy or prior endocrine therapy only (enrollment ongoing).3 The cohort that received a CDK4/6 inhibitor plus AI therapy before second-line treatment with alpelisib plus fulvestrant included 127 patients (median age, 58 years). The primary end point was the proportion of patients alive without disease progression at 6 months per local assessment.
At 6 months post treatment with alpelisib and fulvestrant, 50.4% (95% CI, 41.2%-59.6%) of patients who had previously received a CDK4/6 inhibitor plus an AI were without disease progression. No new safety concerns emerged. The most common AEs included diarrhea (60%), hyperglycemia (58%), nausea (46%), fatigue (29%), decreased appetite (28%), and rash (28%). The most frequent grade 3 or higher AEs included hyperglycemia (28%), rash (9%), and maculopapular rash (9%). Based on these findings, the study investigators, who included Rugo, concluded that alpelisib plus fulvestrant has clinically meaningful efficacy and manageable toxicity after previous treatment with a CDK4/6 inhibitor.3
Oral Taxanes
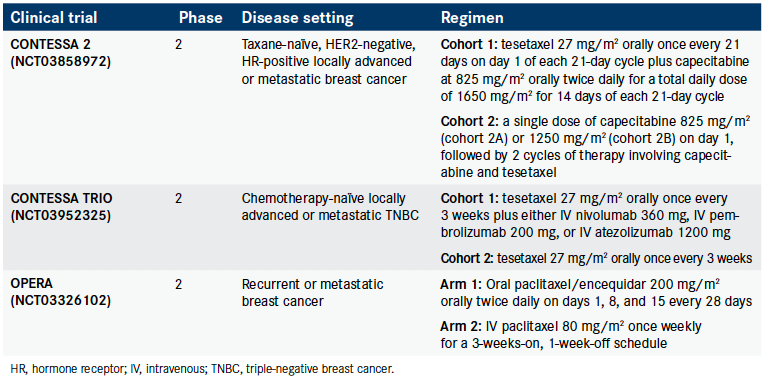
The taxane paclitaxel is a preferred systemic therapy in patients with recurrent or stage IV breast cancer8 but has thus far been available as an IV treatment only. However, several oral taxanes, including tesetaxel and 2 paclitaxel formulations, oral paclitaxel plus encequidar and DHP107 (Liporaxel), are currently in clinical trials testing oral taxanes either alone or in combination with other agents in patients with breast cancer (Table).8-10
Table. Currently Recruiting Clinical Trials of Oral Taxanes in Breast Cancer8-10
The panelists started their discussion of oral taxanes by examining the potential advantages and disadvantages of these treatments, focusing mostly on oral paclitaxel plus encequidar, which had phase 3 data presented at the 2019 San Antonio Breast Cancer Symposium.11 “The perception has been that oral therapy would be simpler and easier for our patients, although I say that is a perception because we’ve found in the space of targeted therapy, that’s not always the case,” Traina said.
One key advantage the panelists noted regarding oral paclitaxel plus encequidar is its potential to reduce trips for patients to receive treatment, which they said may be particularly beneficial during the coronavirus disease-19 pandemic as well as for patients who have to travel long distances to receive care, such as those in rural communities. “Where we are right now in the world, it’s clear that the more that we can get patients away from our infusion units, and the more we can have them have the liberty of getting their treatment at home, that is clearly advantageous,” Isaacs said. However, she added that this advantage needs to be balanced against the toxicities of oral versus IV treatments and the complexity of the regimen, both of which can impede adherence.
The oral paclitaxel plus encequidar regimen is challenging because it has a large pill burden and patients must take it in a certain way. “It comes in a little gelatin capsule, so you need several of them together. Most patients took 10 or 12 tablets each time,” Rugo said. She explained that oral paclitaxel plus encequidar has absorption issues because the intestinal P-glycoprotein efflux pump is clearing the drug as quickly as it is being absorbed, affecting its bioavailability. To prevent this, the regimen adds the agent encequidar, which is a highly specific potent inhibitor of P-glycoprotein that does not have a lot of toxicity on its own. In clinical trials, patients took encequidar as a single tablet before the paclitaxel capsules. The other challenging aspect of the regimen is that it requires periods of fasting.
“You have to wait a certain number of hours after you take 1 aspect of it, then take multiple pills and then fast for more hours. That would raise concerns with some patients, where we do not know whether they would be able to adhere with that complexity,” Sharma said, especially because the regimen is taken 3 days in a row for 3 weeks of an every-4-week cycle. However, she said that oral paclitaxel plus encequidar, unlike IV paclitaxel, does not require the use of weekly steroids, which may be particularly beneficial for patients who have diabetes that is not well controlled. Additionally, the lack of need for steroids enables greater opportunities for pairing this agent with other drugs.
Oral Paclitaxel Phase 3 Study
Investigators studied oral paclitaxel plus encequidar in a phase 3, open-label study conducted in Central America and South America that randomly assigned patients 2:1 to this regimen (n = 265) or IV paclitaxel (n = 137).11 “A lot of these patients had received some prior treatment. About a quarter had received prior chemotherapy, about a third had prior taxane exposure in any setting, and, of course, quite a number had visceral disease, so they were our standard patients,” Rugo said. She explained that the study’s primary end point was tumor response by week 19, which was confirmed 1 month later. She indicated that this end point is different from those traditionally used in registration trials but that it is reasonable because the investigators had to show that oral paclitaxel plus encequidar was at least as good as IV paclitaxel.
The study met its primary end point. For the protocol-defined modified intention-totreat population (baseline evaluable scans and patient received ≥ 75% of the first cycle of dosing), the confirmed response rates were 40.4% for oral paclitaxel plus encequidar and 25.6% for IV paclitaxel (P = .005). “[The investigators] didn’t see big differences in terms of subset analyses. They had the smallest number of patients who had triple-negative disease, so it was a little bit harder to assess in that specific population,” Rugo said. Responses also appeared durable. “About three-quarters of the patients stayed on treatment for more than 100 days and about one-third of patients for more than 200 days, and the follow-up is still ongoing,” she said.
PFS and overall survival, both secondary end points, also favored the oral regimen over IV paclitaxel. In the modified intention-to-treat population, the median PFS was 9.3 months in the oral paclitaxel plus encequidar group compared with 8.3 months in the IV paclitaxel group, with a median overall survival of 27.9 months versus 16.9 months in these groups, respectively.11
Rugo said that one of the most impressive findings was a difference in neuropathy between treatment arms. “If you looked at the grade 2 or greater neuropathy, there was significantly less neuropathy over time with [the oral paclitaxel regimen] compared with IV paclitaxel, a clinically significant difference in terms of developing neuropathy. If you just looked at the total incidence, it was 31% for IV paclitaxel and only 7.6% for the [oral paclitaxel], which is quite different,” she said.
Overall, the toxicity profile of oral paclitaxel plus encequidar was generally similar to that of IV paclitaxel; however, the oral regimen was associated with higher rates of neutropenia, infection, and gastrointestinal AEs. In both treatment arms, the risk of serious AEs was highest in patients with pretreatment evidence of hepatic impairment, and the protocol was amended to address this issue.11
Traina acknowledged the challenges of the study’s design, with the control arm being unusual and the study not providing clarity on certain subgroups. However, she said that she was still encouraged by the neuropathy data. “We have many women who have long-lasting neuropathy because of their adjuvant taxane, and that can be a limiting factor when we need to treat them serially in metastatic disease. To be able to have a taxane that’s active, that has less neuropathy, that perhaps could even partner nicely with some other oral targeted therapies and have a doublet oral regimen, and that enables women to stay out of the infusion suite could be really advantageous,” she concluded.
References
1. FDA approves alpelisib for metastatic breast cancer. FDA. Updated May 28, 2019. Accessed July 9, 2020. bit.ly/2ZdNXVR
2. Andr. F, Ciruelos E, Rubovszky G, et al; SOLAR-1 Study Group. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N Engl J Med. 2019;380(20):1929-1940. doi:10.1056/NEJMoa1813904
3. Rugo HS, Lerebours F, Ciruelos E, et al. Alpelisib (ALP) + fulvestrant (FUL) in patients (pts) with PIK3CA-mutated (mut) hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–) advanced breast cancer (ABC) previously treated with cyclin-dependent kinase 4/6 inhibitor (CDKi) + aromatase inhibitor (AI): BYLieve study results. J Clin Oncol. 2020;38(suppl 15):1006. doi:10.1200/JCO.2020.38.15_suppl.1006
4. Rugo HS, Andr. F, Yamashita T, et al. Alpelisib (ALP) + fulvestrant (FUL) for patients with hormone receptor–positive (HR+), HER2− advanced breast cancer (ABC): management and time course of key adverse events of special interest (AESIS) in SOLAR-1. Ann Oncol. 2019;30(suppl 5; abstr 5535):v104-142. doi:10.1093/annonc/mdz242
5. Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366(6):520-529. doi:10.1056/NEJMoa1109653
6. Novartis gains FDA approval for Afinitor in advanced breast cancer marking a significant milestone for women battling this disease. News release. Novartis. July 20, 2012. Accessed July 9, 2020. http://prn.to/3gHJaBO
7. NCCN. Clinical Practice Guidelines in Oncology. Breast cancer, version 4.2020. Accessed July 9, 2020. bit.ly/2ObUI44
8. Tesetaxel plus reduced dose of capecitabine in patients with HER2 negative, HR positive, LA/MBC.(CONTESSA 2). Clinical-Trials.gov. Updated October 29, 2019. Accessed July 9, 2020. https://clinicaltrials.gov/ct2/show/NCT03858972
9. Tesetaxel plus 3 different PD-(L)1 inhibitors in patients with metastatic TNBC and tesetaxel monotherapy in patients with HER2 negative MBC (CONTESSA TRIO). ClinicalTrials.gov. Updated October 29, 2019. Accessed July 9, 2020. https://clinicaltrials. gov/ct2/show/NCT03952325
10. Oral paclitaxel efficacy safety and PK in recurrent and metastatic breast cancer (OPERA). ClinicalTrials.gov. Updated March 13, 2020. Accessed July 9, 2020. https://clinicaltrials.gov/ct2/show/NCT03326102
11. Umanzor G, Cutler DL, Barrios FJ, et al. Oral paclitaxel with encequidar: the first orally administered paclitaxel shown to be superior to IV paclitaxel on confirmed response and survival with less neuropathy: a phase III clinical study in metastatic breast cancer. Cancer Res. 2020;80(suppl 4):GS6-01. doi:10.1158/1538-7445.SABCS19-GS6-01






















%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
