Publication
Article
Oncology Live®
Prompt Diagnosis Is Vital in Treatment of Tenosynovial Giant Cell Tumors
Author(s):
During an OncLive Peer Exchange®, a panel of orthopedic experts provided a comprehensive overview of these tumors, including their epidemiology and differential diagnosis, optimal clinical workup, and the role of surgical management.
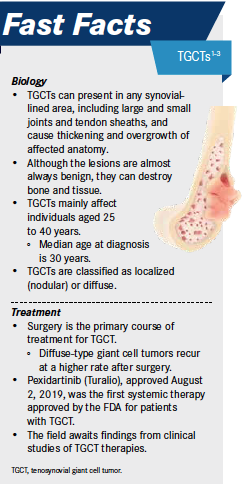
For decades, treatment advances have eluded patients with tenosynovial giant cell tumors (TGCTs), a group of rare tumors that involve the synovium, bursae, and tendon sheath, causing the affected anatomy to thicken and overgrow. Although these lesions are almost always benign, they can be aggressive and destroy the surrounding bone and tissue, making prompt diagnosis and treatment essential to avoiding disability and improving patient outcomes. In 2019, the FDA approved pexidartinib (Turalio), the first systemic treatment for patients with TGCTs that demonstrated a robust tumor response.
During an OncLive Peer Exchange®, a panel of orthopedic experts provided a comprehensive overview of these tumors, including their epidemiology and differential diagnosis, optimal clinical workup, and the role of surgical management. They also discussed the incorporation of pexidartinib into clinical practice and shared their insights on several novel agents in development and future directions in care.
Epidemiology and Differential Diagnosis of TGCT
The terminology used to describe TGCTs has varied in the medical literature. In 2013, the World Health Organization classified these lesions as 2 distinct types of giant cell tumor: giant cell tumor of the tendon sheath and pigmented villonodular synovitis (PVNS).1 “[TGCT] is now recognized as 1 entity…and it can happen in any synovial-lined area, including large joints, small joints, and tendon sheaths,” John A. Abraham, MD, said. He noted that what used to be called PVNS and treated as a separate entity is now known as TGCT of a large joint.
John A. Abraham, MD

TGCTs are rare; Abraham indicated an overall incidence of approximately 30 per million-person years across the disease spectrum. These tumors can be broadly classified as localized (nodular) or diffuse type. The most destructive presentation of TGCTs, the diffuse type that affects large joints, which was previously called PVNS, is even more uncommon, with an overall incidence of 4 to 8 per million-person years. Abraham noted that TGCTs are slightly more common among women and that individuals aged 40 to 60 years are most often affected, though the disease is found across age groups, including in younger patients. “Diffuse disease in the large joints does seem to present in younger age groups—20 to 40 years of age—because that diffuse disease does cause quite a bit of disability, and that younger age group really notices that disability,” he said.
Patients with TGCTs present with inflamed and thickened synovium, a finding that occurs with many other conditions, most oF which are significantly more common than TGCT. Subsequently, the differential diagnosis includes a broad range of conditions that need to be ruled out.1 “One distinguishing factor is that TGCT most commonly will only affect 1 area or 1 large joint. That doesn’t mean it can’t occur in more than 1 place, but we generally see it in 1 place,” Abraham said. When evaluating patients, he said, he listens for comments that suggest a sudden and severe swelling, such as “My knee just blew up.” He noted that such swelling usually results from blood that comes from the thickened synovium and the friable tissue of the synovium, which releases large quantities of blood into the joint and causes symptoms.
Although patients with diffuse disease usually have severe symptoms and those with localized presentations tend to have mild symptoms, Abraham noted that there can be variation in presentations. He has seen mild symptoms in some patients with diffuse disease, as well as significant pain and disability in those with localized disease. “It’s hard to predict what the symptoms will be based on what we see in terms of how much disease is in the joint,” he said.
Although nodular and localized TGCTs are recognized as variants of the same entity, the panelists said they tend to affect different locations. “The nodular types are more consistently found in the extremities such as the hands and feet around tendon sheaths and bursa, and they’re usually localized, solitary nodules,” Tae Won B. Kim, MD, said. “They can have a little bit of a diffuse nature when you look at them with radiology, but overall, they tend to be fairly localized in their distribution. The more symptomatic cases we tend to have more difficulty dealing with are the diffuse type, or cases that occur on a larger joint such as the knee, which is the most common location.” He agreed with Abraham that the symptomology is variable but noted that the diffuse type in larger joints tends to be much more symptomatic. When asked whether localized disease can become diffuse disease, Kim said that he has seen that happen only in the setting of multiple local recurrences following initial resection.
Tae Won B. Kim, MD
Optimal Clinical Workup
“Patient history and physical examination are still your best tools to get to the right diagnosis,” moderator Shreyaskumar R. Patel, MD, emphasized. When considering patients’ history, Abraham said, he listens for phrases suggestive of sudden inexplicable swelling and recurrence, which raise his suspicion of TGCT versus other disorders that present similarly. “The typical things we see [on physical examination] include a very swollen joint, hemarthrosis, or a knee full of fluid, which we would find later to be blood,” he said.
Shreyaskumar R. Patel, MD

Preferred imaging modalities include radiographs and magnetic resonance imaging (MRI). Because radiographs are the least expensive imaging option and provide significant information, Abraham said he starts with that modality. “You may see an effusion on the x-ray. You can see the joint space being expanded,” he said. “There are erosions in the bone that we can see.” However, because radiographs do not show the soft tissue, they do not indicate what is causing these changes, which is where MRI comes in. “The MRI scan gives us a good look at the soft tissue. Synovitis can be seen very well on MRI scans. The T2 scan or fluid-sensitive sequences can show fluid. We can see things like hemosiderin or blood products on T1 imaging. You can see things like blooming artifact,” he said.
Historically, biopsy has not been used to diagnose TGCTs because surgery was the only treatment option; however, with the advent of a systemic treatment, Abraham said a synovial biopsy may be helpful. “With the introduction of systemic therapies for TGCT into the market, it becomes very important to know what we’re treating before we begin medical treatment,” he said, noting that he and his colleagues recently conducted a study and found image-guided synovial biopsy to be safe and effective for establishing a definitive diagnosis of synovial lesions before surgery or other interventions.2
The investigators performed, 54 imageguided biopsies, 36 using computed tomography (CT) and 18 using ultrasonography (US).2 Synovial tissue was obtained in 89% of cases (n = 48), with CT-guided biopsies having a positive yield of 86% and US-guided biopsies having a positive yield of 94%. In 30 cases, surgical pathology was obtained, and the image-guided biopsy concordance was 90%. Of the patients taken for synovectomy, biopsy concordance of suspected neoplastic lesions was 100%. In cases of suspected neoplasm, the concordance between imageguided biopsy and surgical pathology was 96%. No complications were reported.2
Surgical Management of TGCT
“Because of the relatively benign and localized nature of the tumor, surgery has been and will remain the mainstay of therapy,” Patel said.
The panelists noted that to optimally plan surgery, it is essential to know the extent of the TGCT because that will determine the approach. “I usually have the radiologist point out all the areas of disease that I need to address surgically. The goal of surgery is to remove all the diseased synovium,” Abraham said. “We do want a gross total resection. Everything we can see, we would like to get rid of.”
However, Abraham noted, it is often not realistic to remove all disease. “In the knee, for instance, we can probably remove around 85% of the synovium or 90% of the synovium with open surgical techniques. In some of the other joints, it may be less than that. The hip can be particularly difficult because addressing the entire synovium means using a surgical dislocation, which has the potential of being a morbid procedure,” he said.
Some patients may not be candidates for surgery. “If it’s extensive disease that involves the neurovascular bundle with significant erosion into the bone, these may be patients who, right off the bat, we know may not be able to achieve a complete excision,” Abraham said. In such patients, the options need to be weighed, including whether there is any benefit to doing a partial resection or whether systemic treatment should be used.
Kim noted that patients who have had multiple recurrences also might not be good surgical candidates. “On the MRI, it looks as if it’s a fairly reasonable resection to perform, but when you get in there, the only thing you can see is scar tissue around the major structures. Those patients are not the best candidates for up-front surgical resection,” he said.
In rare cases, the surgical approach may necessitate joint replacement or amputation. “Joint replacement is utilized when I feel that the pain is not just tumor related but, rather, that they’ve had a lot of mechanical pain from the joint destruction that you see on the x-ray or MRI,” Kim said. He noted that the need for amputation is rare. “The only times I’ve considered amputation is in the distal extremities, where there’s basically diffuse-type disease in the foot or the hand, where you don’t have soft tissue for coverage, and you know that the morbidity of the surgery is going to be significant. Sometimes a ray resection can be functionally better for the patient than trying to save a finger that’s not salvageable,” he said.
Abraham concurred, noting that amputation may be the best choice for a patient with more aggressive disease with intraarticular/ extraarticular components, compromise of neurovascular bundle, and destruction of the joint.
For patients deemed to be surgical candidates, open resection is preferable to arthroscopic resection, even for localized disease. “When you’re performing an arthroscopic resection, many times what that means is shaving the tumor down. We know, based on the mechanism of how this works, that there is a paracrine loop where 1 tumor cell is sending out a signal that is then recruiting cells into the normal synovium. Shaving that down and spreading that tissue everywhere is probably not a great idea,” Abraham said. He noted that in some cases a mini-arthrotomy can be performed, including most locations in the knee. “[You] make a very small opening and get to the lesion and remove it. That has a very minimal change in functional recovery versus an arthroscopic procedure,” he said. If there is posterior disease, the tumor is otherwise difficult to access, or extensive dissection is needed, Abraham said he will discuss the case with his arthroscopic colleagues to better plan the surgical approach.
Advent of Systemic Treatments: Pexidartinib and Beyond
On August 2, 2019, the FDA approved pexidartinib, a selective tyrosine kinase inhibitor (TKI) against the colony-stimulating factor receptor (CSF1R), marking approval of the first systemic therapy to treat TGCT.3 FDA approval was based on the 2-part ENLIVEN trial (NCT02371369).4 The first part was a double-blind study in which symptomatic patients who were not candidates for surgery were randomly assigned 1:1 to pexidartinib (n = 61) or placebo (n = 59) for 24 weeks, with a loading dose of pexidartinib 1000 mg orally daily given the first 2 weeks, followed by 800 mg orally daily given for the next 22 weeks. The second part was an open-label study of pexidartinib for all patients. The primary end point, assessed in all intention-to-treat patients, was overall response at week 25 and was centrally reviewed by RECIST v1.1.
Gina Z. D’Amato, MD

“The overall response rate by RECIST criteria was 38% versus 0% in the placebo group, with a 15% complete response rate, which is really astounding. About 80% of these patients were on it for more than 6 months, and two-thirds were on it for over a year,” Gina Z. D’Amato, MD, said. She noted that by tumor volume, the response rate was 56%.
Another remarkable finding was that almost all patients who received pexidartinib had some degree of tumor shrinkage. “There was practically no one who had tumor growth on this drug, so that was quite striking. That speaks to how even with smaller degrees of shrinking, people can have symptomatic improvement, as well,” Robert G. Maki, MD, PhD, said.
Robert G. Maki, MD, PhD

A challenge with pexidartinib, however, is its adverse effect (AE) profile. Although the treatment is generally well tolerated, Maki said that because this tumor is not cancerous, the FDA has set a much higher safety bar. “We have to be very careful about watching for things like transaminitis and elevations of LFTs [liver function tests] in these patients,” he said. In the ENLIVEN trial, serious AEs occurred in 8 (13%) of the 61 pexidartinib-treated patients, with increases in aspartate aminotransferase (AST) and alanine aminotransferase (ALT) occurring in 39% and 28% of patients, respectively.4
Three pexidartinib-treated patients had AST or ALT elevations 3 or more times the upper limit of normal, with total bilirubin and alkaline phosphatase 2 or more times the upper limit of normal, suggesting mixed or cholestatic hepatotoxicity. Because of the increase in LFTs, pexidartinib is prescribed under a risk evaluation and mitigation strategy [REMS] that requires regularly monitoring patients for LFT abnormalities, including before initiating treatment, weekly for the first 8 weeks, every 2 weeks for the next month, and then once every 3 months.3 “[LFT elevations] can be mitigated by stopping the medication for a little while and then restarting it, and reducing the dose depending on recurrence,” Maki said.
Other AEs commonly observed with pexidartinib included hair color changes (67%), fatigue (64%), nausea (38%), eye edema (30%), rash (28%), and dysgeusia (26%).4,5 Maki said the hair color changes occur because pexidartinib is a good KIT inhibitor. “KIT is involved in pigmentation, so people have their hair turn white or at least lighter tone, and it can affect their skin tone, as well. That can be disconcerting for some people,” he said.
Using Pexidartinib in Clinical Practice
In most cases, patients with TGCTs are primarily treated by orthopedic surgeons, who have not previously had any medical treatments available. Although Abraham said he obtained the certification for the pexidartinib REMS program, he does not plan to prescribe this drug but wanted to learn more about it and how patients respond. “My approach is, if I have a patient who I don’t think is surgically resectable or is multiply recurrent and I think it is a good idea to put them on the drug, I would then send them to a medical oncologist,” he said.
Kim said he makes sure to discuss the drug with his patients who have diffuse TGCTs. “I always [introduce] the idea that we’ve got this treatment option that’s on the table. It may not necessarily be right now that it’s necessary, but at least if they are well educated on it, when I do send them to medical oncologist, they can have a more fruitful discussion regarding it,” he said.
Agents in Clinical Trials
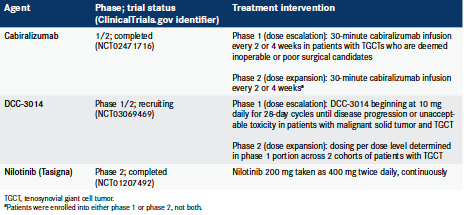
The panelists noted that pexidartinib is just the start of systemic treatments for TGCTs and that several agents are in clinical trials, including an antibody called cabiralizumab and a small molecule known as DCC-3014 (Table).6,7 Outcomes data are not yet available from these studies. Nevertheless, Patel said, these clinical trials “will broaden the horizons and give us a little bit of perspective on what would be the best sequence and way to incorporate these drugs.”
Table. Investigational Agents for the Treatment of TGCTs6,7
Maki noted that one area that will require research but offers additional promise involves using systemic treatments in neoadjuvant settings. “It brings out this idea that if you are treating someone who’s presenting relatively early in their course, and it’s diffuse disease around the knee or the hip, you can propose neoadjuvant approach first using pexidartinib and then surgery. Will that be better than just doing the surgery up front and waiting for people to recur? All these will be interesting research topics,” he said.
Conclusions
In their concluding remarks, the panelists agreed that surgery remains the cornerstone of treatment but medical therapy is enabling treatment for patients who previously had no options. They emphasized the importance of following a multidisciplinary approach to care, including surgery, radiology, pathology, and medical oncology, so that the full range of options can be investigated for each patient, particularly those with diffuse disease.
“As a surgeon dealing with this frequently, my closing message is: First, recognize that the disease exists and know how to diagnose it. Second, send patients to the right place to treat it. Third, be aware that there is a medical therapy that has proved thus far to be very good at controlling symptoms and bulk from this disease,” Abraham said.
- Tenosynovial giant cell tumor. National Organization for Rare Disorders. 2017. Accessed August 13, 2020. https://rarediseases.org/rare-diseases/tenosynovialgiant-cell-tumor/
- McKee TC, Belair JA, Sobol K, Brown SA, Abraham J, Morrison W. Efficacy of image-guided synovial biopsy. Skeletal Radiol. 2020;49(6):921-928. doi:10.1007/s00256-019-03370-2
- FDA approves pexidartinib for tenosynovial giant cell tumor. FDA. August 2, 2019. Accessed August 13, 2020https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-pexidartinib-tenosynovialgiant-cell-tumor
- Tap WD, Gelderblom H, Palmerini E, et al. Pexidartinib versus placebo for advanced tenosynovial giant cell tumour (ENLIVEN): a randomised phase 3 trial. Lancet. 2019;394(10197):478-487. doi:10.1016/S0140-6736(19)30764-0
- Turalio. Prescribing information. Daiichi Sankyo, Inc; 2019. Accessed August 13, 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/211810s000lbl.pdf
- Study of cabiralizumab in patients with pigmented villonodular synovitis / diffuse type tenosynovial giant cell tumor (FPA008-002). ClinicalTrials.gov. Updated July 31, 2020. Accessed August 13, 2020. https://clinicaltrials.gov/ct2/show/NCT02471716
- Study of DCC-3014 in patients with advanced tumors and tenosynovial giant cell tumor. ClinicalTrials.gov. Updated May 5, 2020. Accessed August 13, 2020. https://clinicaltrials. gov/ct2/show/NCT03069469




























%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
%20(2)%201-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered-Recovered.jpg?fit=crop&auto=format)
