Publication
Article
Oncology Live®
Shortage of Cancer Care Providers in Rural Areas Affects Patient Outcomes
Author(s):
In the United States, a geographic mismatch exists between the number of medical oncology and radiation providers and patients needing care, with more specialists clustered in urban and metropolitan areas.
Smita Bhatia, MD, MPH

In the United States, a geographic mismatch exists between the number of medical oncology and radiation providers and patients needing care, with more specialists clustered in urban and metropolitan areas. This imbalance happens, investigators said, because of the infrastructure needed to support high-quality oncology care. Larger geographic areas offer access to hospitals and universities, clinical trials, peers, and centers that furnish radiation services.
Addressing the gap in providers in rural areas is important because it affects patient care, experts say. Cancer incidence rates and deaths are higher in rural areas than in metropolitan areas.1 One analysis published in 2017 looked at 5-year cancer incidence and mortality rates between 2009 and 2013. Investigators found that in metropolitan counties, cancer incidence was 447 cases per 100,000 people, (range, 446-456 depending on county characteristics), whereas in rural counties, the incidence was 460 per 100,000 (range, 439-477).
Mortality rates were 166 per 100,000 in metropolitan counties (range, 164-173) and 182 per 100,000 in rural counties (range, 174-185). The difference was statistically significant for both benchmarks (P < .001).1
“Access to oncology services is impacted by the low density of oncologists in the rural settings,” Smita Bhatia, MD, MPH, director of the Institute for Cancer Outcomes and Survivorship at the University of Alabama at Birmingham (UAB) School of Medicine, said in an interview with OncologyLive®.
She is also vice chair for outcomes in the Department of Pediatrics and associate director for outcomes research of the UAB Comprehensive Cancer Center, and associate director of the Center for Outcomes and Effectiveness Research and Education.
“We know that if patients with cancer who are undergoing treatment aren’t carefully monitored, they may have [adverse] effects or an exacerbation of symptoms, or other things that could go wrong. Then when the situation really deteriorates, they may go to emergency departments,” Susan Dentzer, senior policy fellow for Robert J. Margolis Center for Health Policy at Duke University in Durham, North Carolina, said in an interview.
GEOGRAPHIC IMBALANCE
Susan Dentzer

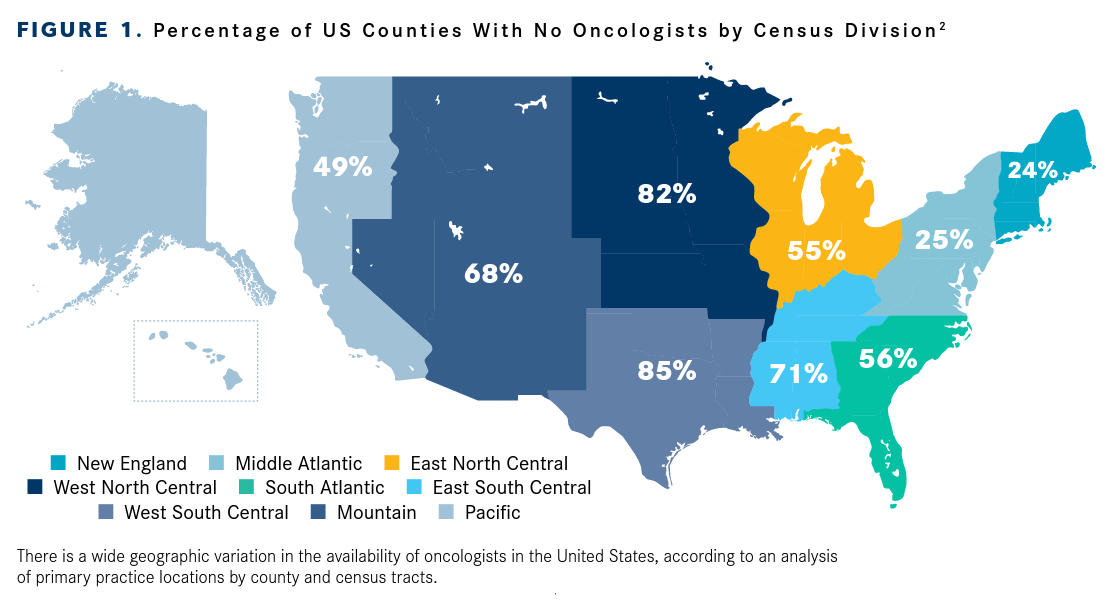
In 2019, 64% of US counties had no oncology care providers whose primary practice site was within that county, and 12% had no oncologists in the adjacent counties, according to a recent analysis in JCO Oncology Practice.2
Investigators in this study looked at the geographic distribution of oncologists and oncology pharmacists registered in the 2019 National Provider Identifier database and found wide discrepancies in the number of oncologists across geographic regions.
More than 65% of oncologists were based in 4 of 9 US Census Bureau divisions; areas with the fewest oncologists were located in the West North Central and West South Central divisions (FIGURE 12). Of note, a lower availability of cancer care providers was negatively associated with higher cancer rates (correlation, -0.085; P < .01).2
Another analysis conducted by the American Society of Clinical Oncology (ASCO) showed that just 403 of the 1698 US hematology and medical oncology practices listed in the CMS Physician Compare database have sites in rural areas.3
David Beyer, MD

Almost 9 in 10 radiation oncologists work in urban or suburban communities (47% and 41%, respectively). The proportion of those practicing in rural areas declined from 16% in 2012 to 13% in 2017, according to the American Society for Radiation Oncology (ASTRO).4
Meanwhile, the percentage of the US population living in rural areas varies from 15% to 19%, depending on the definition used. The US Census Bureau, for example, doesn’t actually define “rural.” It classifies Urbanized Areas as those with 50,000 or more people and Urban Clusters as those with 2500 to fewer than 50,000 people.
In the 2010 Census, 59.5 million people, 19.3% of the population, were considered to be living in rural areas, and more than 95% of US land area is still classified as rural.5
The Office of Management and Budget (OMB) considers all areas outside of a metropolitan statistical area as rural. In 2010, non-metropol-itan counties contained 46.2 million people, approximately 15% of the total population and covered 72% of the land area of the country.
The Federal Office of Rural Health Policy uses the OMB classification but uses an addi-tional measure that attempts to allow for better identification of rural areas. By this measure, 57 million people, approximately 18% of the population, and 84% of the nation’s land area are considered rural.
FIGURE 1. Percentage of US Counties With No Oncologists by Census Division
TACKLING GAPS IN CARE
ASCO and ASTRO have implemented initia-tives to focus on oncology care in rural areas. In 2019, both organizations launched efforts to address the needs of oncology care providers in rural areas and better support oncologists regarding provider education and training, telehealth, and research3 (FIGURE 26).
Bhatia, who is on ASCO’s cancer care task force, said the organization has developed recommendations for addressing oncology care and supporting rural oncologists; these are in manuscript form and will be published soon. One recommendation, she said, is to increase education, training, and mentoring opportunities for those practicing in rural areas, as well as develop the workforce development and build capacity.
Geraldine M. Jacobson, MD, MPH, MBA, FACR, FASTRO

Continuing education for physi-cians and staff has always been an issue in rural areas, said David Beyer, MD, medical director of radi-ation oncology at Cancer Centers of Northern Arizona Healthcare in Sedona. “The COVID-19 pandemic has forced us to exper-iment. A lot of CME [continuing medical education] last year was virtual, and it may be that we discovered quite by accident the models that might work in the future.”
The ASCO task force also recom-mended the following: harnessing the growing quality improvement and practice health programs to improve cancer care delivery in rural settings; collecting and analyzing additional data to better understand the current state, needs, and challenges of the rural cancer care workforce in both oncology and nononcology; and promoting research of the design and implementation of cancer care delivery models in the rural setting, Bhatia said in an interview.
Building up the oncology work force in rural areas will require making changes to training programs, said Geraldine M. Jacobson, MD, MPH, MBA, FACR, FASTRO, a radiation oncologist, professor and chair of the Department of Radiation Oncology at West Virginia University Cancer School of Medicine in Morgantown, West Virginia.
One way to do this would be to invest in a national program that supports physicians who want to practice in rural communities. “We need to get people from rural areas into our medical pipeline who will practice in rural areas and that includes maintaining our smaller training programs,” she said in an interview. “Money follows money and technology follows technology. If we want a different outcome, we have to do something different.”
FIGURE 2. ASCO’s Plan to Support Oncology Providers in Rural Areas
A DIFFERENT MODEL IS NEEDED
Capacity building and increasing the density of oncology providers and ancillary support staff is important, but that won’t entirely address the rural care issues, Dentzer said.
A different model of care for patients is needed, where they are supported in their homes with telehealth services from clinicians and visits from advanced practice providers. Even in less populous states such as New Mexico, oncologists generally practice in urban or suburban areas, and it’s unlikely they will move to outlying areas, she noted.
“The business model for them [to operate in rural areas] would be unsustainable for the most part. It’s just not going to happen. We focus too much on getting patients and specialists in the same room. The question becomes how to get patients and specialists’ knowledge in the same room. And we’ve found we can put people together via technologies and via telehealth. It’s not about people transfer; it’s about knowledge transfer.”
Dentzer pointed to Project ECHO, the now-global effort that originated at the University of New Mexico School of Medicine as an example.
Project ECHO—which stands for Extension for Community Healthcare Outcomes—began in 2003 as a model to help specialists at the University of New Mexico in Albuquerque support primary care doctors and other clinicians in outlying areas of the state in treating treat patients with hepatitis C. Project ECHO has since grown to include global initiatives in many disease areas, including HIV, tuberculosis, rheumatology, maternal health, and opioid use disorders, as well as oncology.7
Oncology organizations are beginning to launch similar efforts. One is ASTRO’s Peerto-Peer Match, which was released in June 2020. The online platform facilitates relationships and connects ASTRO members for peer review of patient cases. It allows clinicians to search for those with similar expertise to assist in evaluating treatment plans.8
Peer-to-Peer Match helps to address a challenge radiation professionals in rural areas face, Beyer said. “This program is essentially a ‘Match.com’ for radiation oncologists in rural settings who want to review plans with somebody else, someone who has a similar practice style, a similar practice size, similar technical capabilities.”
Rural oncology patients can also be served by “hospital-at-home” programs, Dentzer said. An example of one such program is Huntsman at Home offered by Huntsman Cancer Institute at the University of Utah in Salt Lake City.
The institute launched Huntsman at Home in 2018 to support patients and caregivers and manage acute and post-surgical care, as well as end-of-life care. It uses nurse practitioners and registered nurses, working with oncology teams, to deliver acute level care at home.9
An evaluation of the program’s utilization outcomes was presented at the 2020 ASCO Virtual Scientific Program. Investigators found evidence that the Huntsman at Home program can improve value by reducing hospitalizations, emergency department visits, and costs.
Investigators focused on patients at hospital discharge who needed continued acute level care. They found that for the first 14 months of the program, 19.5% of patients in Huntsman at Home (n = 169) had 1 or more unplanned hospitalizations compared with 35.4% of patients in a similar group outside the 20-mile radius of the hospitals (n = 198).10
Additionally, 14.2% of Huntsman at Home patients had 1 or more emergency department visits vs 23.2% for the comparison group. Mean costs were also lower in the Huntsman at Home group ($10,238) vs the usual care group ($21,363).
“This was an initial test of the concept in oncology, and it shows that extending acute level cancer care into the home and communities of cancer patients utilizing a hospital-at-home model can significantly improve patient experience and outcomes,” said Kathi Mooney, PhD, RN, who presented the results. Mooney is a distinguished professor at the University of Utah College of Nursing and coleader of the Cancer Control and Population Sciences Program at the Huntsman Cancer Institute.
Currently, the program is available to patients within a 20-mile radius of the hospital in Salt Lake City. Hospital administrators are also working to increase Huntsman at Home’s reach, extending care to several rural counties in the state. In July 2020, Huntsman Cancer Institute received a $4.5 million gift from the Huntsman family to expand the program to rural Utah.11
The institute is in the planning process for expanding the program to Carbon, Grand, and Emery counties, working with the communities identified for the rural expansion and the Huntsman Cancer Institute clinical teams, according to a Huntsman spokesperson. These counties were selected following evaluation of Utah’s cancer burden and conversations with community organizations and elected officials in these areas.
References
- Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and future trends. Cancer Epidemiol Biomarkers Prev. 2017;26(7):992-997. doi:10.1158/1055-9965.EPI-17-0092
- Shih YCT, Kim B, Halpern MT. State of physician and pharmacist oncology workforce in the United States in 2019. JCO Oncol Pract. 2021;17(1); e1-e10. doi:10.1200/OP.20.00600
- Key trends in tracking supply of and demand for oncologists. American Society of Clinical Oncology. August 2020. Accessed March 25, 2021. https://bit.ly/2RwnopZ
- Radiation oncology workforce study indicates potential threat to rural cancer care access. News release. Newswise. April 4, 2019. Accessed March 25, 2021. https://bit.ly/3sp3azg
- Defining rural population. Health Resources and Services Administration. Updated January 2021. Accessed March 25, 2021. http://bit.ly/3fbKUFN
- ASCO announces new task force to address rural cancer care gap. News release. American Society of Clinical Oncology. April 10, 2019. Accessed March 25, 2021. http://bit.ly/3d5Gbmy
- Project ECHO. University of New Mexico. Accessed March 25, 2021. https://hsc.unm.edu/echo/
- Beyer D. Introducing Peer-to-Peer Match, a new platform for radiation oncologists. ASTRO blog. June 2, 2020. Accessed March 25, 2021. https://bit.ly/39fIvGq
- Huntsman Cancer Institute researchers demonstrate better outcomes, lower cost in first-ever oncology hospital at-home evaluation. Huntsman Cancer Institute. May 29, 2020. Accessed March 25, 2021. http://bit.ly/2PBeQ3E
- Mooney K, Titchener K, Haaland B, et al. The oncology hospital at home: health care utilization outcomes from the Huntsman at Home trial. J Clin Oncol. 2020;38(suppl 15):7000. doi:10.1200/JCO.2020.38.15_suppl.7000
- Huntsman Cancer Institute announces next major expansion: cancer care coming to patient home in rural Utah. Huntsman Cancer Institute. July 15, 2020. Accessed March 25, 2021. http://bit.ly/3m2kOqr