Publication
Article
Contemporary Oncology®
The Clinical and Economic Value of Rituximab for the Treatment of Hematologic Malignancies
Rituximab is a humanized monoclonal antibody that is used for the treatment of a wide variety of B-cell-derived hematologic malignancies
Abstract
Rituximab is a humanized monoclonal antibody that is used for the treatment of a wide variety of B-cell—derived hematologic malignancies, including follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL), the 2 most commonly occurring subtypes of non-Hodgkin lymphoma, as well as chronic lymphocytic leukemia (CLL). Multiple studies show that rituximab improves clinical outcomes and is a cost-effective therapy for FL, DLBCL, and CLL. Recent results from the PRIMA study have demonstrated that rituximab as maintenance therapy prolongs the duration of response and significantly reduces the risk of progression. Rituximab continues to undergo active clinical investigation to optimize survival outcomes and safety in both initial treatment and maintenance settings, as well as in combination with other targeted therapies. We review the clinical evidence demonstrating the efficacy, safety, and cost of rituximab in the treatment of B-cell–derived diseases and discuss ongoing avenues of investigation of the drug.
Since US Food and Drug Administration (FDA) approval in 1997, rituximab (Rituxan) has been one of the most widely prescribed biological agents in the United States.1 The ubiquitous expression of the target protein CD20 on the surface of B lymphocytes and the fact that the vast majority of non-Hodgkin lymphomas (NHLs) are B-cell malignancies have provided the rationale for the development of this humanized monoclonal antibody, which has become one of the most commonly used therapeutic agents for this group of malignancies.2-5
In combination with chemotherapy, rituximab significantly improves survival outcomes for patients with follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL), the 2 most commonly diagnosed subtypes of NHL.6-11 Rituximab as maintenance therapy has been shown to significantly reduce the risk for progression in patients with newly diagnosed and relapsed FL.12,13 Further, chemoimmunotherapy-containing rituximab significantly improves complete response (CR), progression-free survival (PFS), and overall survival (OS) rates for patients with either previously untreated, relapsed, or refractory chronic lymphocytic leukemia (CLL).14,15 Based on such efficacy data, rituximab is FDA-approved for the treatment of FL, DLBCL, and CLL in a number of settings.16 Importantly, studies show rituximab to be a cost-effective treatment with a very favorable toxicity profile and reduced needs for ancillary medical care.17-21 We review the clinical evidence supporting the benefits and safety of treatment with rituximab, the costeffectiveness of the therapy, and continued clinical investigation to optimize outcomes and increase convenience of use.
Treatment
Aggressive/Diffuse Large B-Cell Lymphoma
Untreated Disease. Rituximab, combined with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) chemotherapy (R-CHOP), is the only approved biologic agent reported to significantly improve survival rates for a broad range of patients with untreated DLBCL, including both the young and the elderly, as demonstrated in 3 large-scale clinical trials.10,11,22 Both the LNH 98-5 and E4494 trials were conducted in untreated patients who were 60 years and older.11,22
Long-term follow-up after 10 years in the LNH 98-5 study showed treatment with R-CHOP continued to result in a significant survival benefit (43.5% vs 27.6%; P <.0001).11 The median PFS from this latest analysis was 8.4 years for R-CHOP compared with 3.5 years for CHOP alone. Significant improvements in the 10-year PFS (36.5% vs 20.1%, P <.0001), event-free survival (EFS) (34% vs 19%, P <.001), and disease-free survival (64.5% vs 42.6%, P <.001) rates also were observed. In the E4494 trial similar improved clinical benefits were observed with R-CHOP (3-year time to treatment failure and OS measures) compared with CHOP alone.22 Both trials demonstrated that improved clinical benefits were maintained across all analyzed subgroups. Six-year follow-up results from the phase III MInT trial conducted in 834 younger (≤60 years) patients who had a favorable prognosis and were treated with rituximab in combination with CHOP or CHOP-like chemotherapy showed significantly improved 6-year EFS and OS rates compared with CHOP or CHOPlike chemotherapy alone (74% vs 56%, P <.001; 90% vs 80%, P = .001, respectively).10
There is evidence that bcl-6—positive patients may have similar outcomes with R-CHOP or CHOP, suggesting that bcl-6–positive patients may not benefit from rituximab added to CHOP. A prospective correlative study of patients from the Intergroup phase III trial showed that no differences in failure-free survival and OS were detected between treatment arms for bcl-6–positive cases.23
Relapsed or Refractory Disease. The role of rituximab in the treatment of patients with relapsed aggressive lymphomas continues to be investigated. Salvage chemotherapy followed by high-dose therapy and autologous stem cell transplantation is the standard of treatment for patients with chemosensitive relapses of DLBCL. Clinical results to date suggest that various applications of rituximab therapy may improve outcomes in several ways for those patients: in combination with chemotherapy prior to autologous stem cell transplantation, as single-agent therapy following autologous stem cell transplantation, and in combination with other drugs for patients ineligible for transplantation.24-26 Investigators have reported that the addition of rituximab to ifosfamide, etoposide, and carboplatin (R-ICE) significantly increased the CR rate, using historical comparison with ICE alone (54% vs 27%).25 Further, 2 single-arm studies of the dexamethasone, cytarabine, and cisplatinum plus rituximab (R-DHAP) and DHAP regimens showed overall response (OR) and CR rates of 82% versus 56% and 33% versus 31%, respectively.27,28
The phase III CORAL trial randomized patients with relapsed or refractory DLBCL to receive rituximab and either ICE or DHAP chemotherapy, followed by autologous stem cell transplantation and maintenance rituximab therapy, administered every 2 months for 1 year in responding patients.24 The OR rate was 63% (CR 38%), with no difference between R-ICE (63.5%) and R-DHAP (62.8%). Similarly, no (26% vs 35%) and OS (47% vs 51%) rates between R-ICE and R-DHAP, respectively. Rituximab-containing salvage therapy resulted in an 83% response rate in patients who had not previously received rituximab.24 The results from responding patients randomized to maintenance therapy are awaited.
Chronic Lymphocytic Leukemia
A fludarabine plus cyclophosphamide regimen (FC) to which rituximab was added (FCR) was clinically proved to significantly improve the OR, CR, and PFS rates and the OS outcomes that were gained from chemotherapy alone, for patients with either previously untreated or relapsed CLL.14,15,29-33
Untreated Disease. Long-term follow-up results from 300 patients with previously untreated disease who received FCR showed OR, CR, and 6-year survival rates of 95%, 72%, and 77%, respectively.31 For untreated patients with CLL, the superiority of FCR over FC has been demonstrated recently in a large randomized trial.14 The phase III CLL8 study, with 817 enrolled patients, showed those who received FCR had a higher OR rate (FCR 90% vs FC 80%) and significantly increased CRs (FCR 44.1% vs FC 21.8%, P <.0001). With a median follow-up of 37.7 months, the median PFS was significantly increased (51.8 months with FCR compared with 32.8 months with FC alone; hazard ratio [HR] = 0.56, P <.0001). A statistically significant improvement in the 3-year OS rate was observed with FCR (87.2% vs 82.5%; HR = 0.664, P = .012). The median survival has not yet been reached in either treatment arm.14 Further, the improved PFS and OS benefit with FCR was observed across the majority of patient subgroups analyzed.14,34
Binet stage C patients had a shorter PFS benefit compared with Binet stage A and B patients, and did not show an improvement in the OS rate with FCR.14 Subgroup analyses for poor-risk cytogenetic markers showed that FCR was superior to FC for complete remissions in the following groups: 11q deletion (53.2% vs 15.5%, P <.001); unmutated IGVH (42.9% vs 20.4%, P <.001); trisomy 12 (70.8% vs 21.9%, P <.001); and 13q single deletion (49% vs 24.8%, P <.001), respectively.34
With regard to safety, grade 3 or higher adverse events that occurred more often with FCR included hematologic toxicity (55% vs 39%), neutropenia (33.7% vs 20.9%), and leukocytopenia (24% vs 12.1%).14 The increase in the rate of neutropenia did not result in an increased infection rate (18.8% for FCR and 14.8% for FC). In both the CLL8 trial and the REACH trial (see Relapsed and Refractory Chronic Lymphocytic Leukemia below), rituximab was dosed at 375 mg/m2 for cycle 1 and then at the higher dose of 500 mg/m2 for cycles 2 through 6. The rationale for this increase in rituximab dose is based on pharmacokinetic data that showed the clearance rates for the drug are higher in general for patients with CLL compared with NHL, possibly due to higher numbers of circulating malignant CLL cells.35
Relapsed and Refractory Chronic Lymphocytic Leukemia. Improved clinical outcomes with FCR treatment also extend to patients with relapsed or refractory CLL. A retrospective analysis by MD Anderson Cancer Center researchers of 505 previously treated patients showed FCR had a higher CR rate (fludarabine 13%, FC 12%, FCR 28%) and significantly increased survival (median survival: fludarabine 19 months; FC 31 months; FCR not yet reached).32 An open-label study of 177 patients treated with FCR also demonstrated high response rates (OR 73%, CR 25%), with median time to progression and OS of 28 months and 42 months, respectively.33 The large phase III study REACH compared FCR and FC regimens in 552 patients with relapsed or refractory CLL and found that median PFS was significantly increased in the FCR arm (30.6 months vs 20.6 months, P = .0002).15 Overall responses (70% vs 58%, P = .0034) and CRs (24% vs 13%, P = .0007) were significantly higher in the FCR arm compared with the FC arm. The median OS has not yet been reached for FCR and was 53 months for FC.15 The results for FCR were consistent across secondary end points (EFS, time to next treatment, and duration of response) and in most patient subgroups with adverse prognostic features (Binet C stage disease, chromosome 11q deletion, unmutated IgVH gene, ZAP-70 positive B-CLL cells).15
No new or unexpected toxicity was seen in the REACH trial, and the FCR combination showed a favorable risk-benefit profile. Adverse events were seen in 80% of patients in the FCR group and 74% in the FC group, and serious adverse events were seen in 50% and 48%, respectively.15 The most common adverse events that occurred more often in the FCR arm included blood and lymphatic system disorders, infections, and neoplasms. Grade 3 or higher neutropenia was comparable between the 2 arms (FCR 42% vs FC 40%), as was febrile neutropenia (FCR 12% vs FC 12%).15 Rates of grade 3/4 thrombocytopenia (FCR 11% vs FC 9%) and grade 3/4 infections (FCR 18% vs FC 19%) were similar. A slightly higher rate of fatal adverse events was seen with FCR (14%) compared with FC (10%).15
Follicular Lymphoma
Initial Therapy. Follicular lymphoma is considered to be incurable with standard chemotherapeutic options.36 Multiple randomized phase III trials show treatment with rituximab, in combination with different chemotherapy regimens, resulted in significantly prolonged OS rates for patients with FLs compared with chemotherapy alone.6,7,37,38 Further, the trials investigating the R-CHOP and cyclophosphamide, vincristine, and prednisone plus rituximab (R-CVP) regimens showed the clinical improvements were maintained across all analyzed subgroups, including patients with low- or high-risk profiles, patients younger than 60 years, and patients 60 years and older.6,7
Rituximab continues to be studied in combination with new agents with the goal of improving outcomes and patient safety. Recently, the phase III StiL trial compared the regimen of rituximab plus bendamustine (BR) with R-CHOP.39 The CR rate was significantly better for BR (40.1% vs 30.8%, P = .0323), as were the median PFS (54.8 vs 34.8 months; HR = 0.5765, P = .0002) and median EFS (54 vs 31 months; HR = 0.6014, P = .0002).39 The safety profile of the BR regimen is also improved and was associated with fewer serious adverse events (BR, n = 49 vs R-CHOP, n = 74) and significantly lower rates of grade 3/4 neutropenia (10.7% vs 46.5%; P <.0001) and grade 3/4 leukocytopenia (12.1% vs 38.2%; P <.0001). Growth factor (G-CSF) was used more often used in R-CHOP treated patients (20% vs 4.0% of all cycles for BR).39
Therapy for Relapsed or Refractory Follicular Lymphoma. Given the incurable nature of FL, treatment options are limited once the patient relapses after initial therapy. Chemoimmunotherapy with rituximab has improved survival outcomes for patients with relapsed or refractory FL. In a phase III study, 465 patients received randomized treatment with R-CHOP or CHOP alone.9 The CR rate was significantly superior for the R-CHOP—treated group (29.5% vs 15.6%). The median PFS and the 3-year OS rates also were better for those patients receiving R-CHOP (Figure 1). A second randomized phase III trial showed that rituximab plus fludarabine, cyclophosphamide, and mitoxantrone (R-FCM) also significantly improved CRs, median PFS, and 2-year survival rates compared with FCM alone.8 R-FCM was also superior to FCM in all analyzed subgroups, including patients who had received 1 prior therapy (OR 82% vs 71%), those who had received 2 or more prior therapies (OR 74% vs 41%), and those identified as having disease refractory to prior therapy (OR 62% vs 20%). A similar survival benefit was observed when results were analyzed for those patients with recurrent FL (2-year OS rate 90% vs 70%).8
Rituximab as Maintenance Therapy in Follicular Lymphoma. Patient retreatment with maintenance rituximab following a response to initial therapy has been shown to be effective in extending the duration of remission.40 The optimal timing and dosing schedules have not yet been elucidated, but to date all of the various dosing schedules have resulted in improved patient outcomes. These include once every 2 months, once every 3 months, or a once-weekly dose for 4 weeks every 6 months, for a period up to 2 years after initial induction therapy.9,41,42 In these trials, patients experienced a survival benefit from maintenance rituximab regardless of the chemotherapy regimen (FCM, CVP, CHOP) used as induction therapy, whether the patients had been previously treated or not, or whether rituximab was included as part of induction therapy.9,41-44 In the phase III ECOG 1496 trial with treatment-naïve patients, maintenance rituximab following initial CVP induction significantly prolonged PFS (median 51.6 vs 15.6 months, P = 4.4 x 10-10) and increased the 3-year OS rate (91% vs 86%, P = .08) in a group of 311 patients, including 282 with FL.41 This improvement in PFS was maintained across all patient subgroups.41 The SAKK 35/98 trial showed the median EFS was almost doubled for maintenance rituximab and that 25% of the patients receiving maintenance rituximab were still in remission at 8 years. A subanalysis of the chemotherapy-naïve patients showed an even greater benefit with maintenance rituximab; approximately 45% were in remission at 8 years.42 The efficacy and safety of maintenance rituximab also are being investigated in the ongoing phase IIIb MAXIMA trial.45 This trial has enrolled 545 patients with either untreated FL (72.8%) or relapsed FL (27.2% with 2 or more treatments). More than two-thirds (69.7%) of the patients entered the study with a CR/unconfirmed CR (CRu) and the remainder had a partial response (PR) from their most recent treatment. At a median follow-up of 28.8 months, 92.6% of 381 patients with a post-induction CR/Cru remained in CR/ Cru during maintenance. Eleven (6.7%) patients with a PR converted to CR after maintenance.45
Results from the phase III PRIMA (Primary Rituximab and Maintenance) study have confirmed the clinical benefits of using maintenance rituximab in the front-line setting.12 This trial, with 1217 enrolled patients, randomized patients responding to induction immunochemotherapy consisting of either 8 cycles of R-CVP, or 6 cycles of R-CHOP or R-FCM (plus 2 additional rituximab infusions), to maintenance rituximab or observation. After a median followup of 36 months, 3-year PFS rates were 74.9% and 57.6% in the maintenance rituximab and observation arms, respectively.12 Maintenance rituximab significantly prolonged PFS for patients who responded to induction with R-chemotherapy induction, reducing the risk for disease progression by 45% (HR = 0.55, P <.0001). The benefit from maintenance was observed regardless of the induction regimen (R-CHOP, HR = 0.51; R-CVP, HR = 0.68; and R-FCM, HR = 0.54), age of the patient (<60 years, HR = 0.49; ≥60 years, HR = 0.67), and the response to induction (CR/Cru, HR = 0.57; PR, HR = 0.48).12 Patients treated with maintenance rituximab also had significantly longer time to next treatment (HR = 0.60, P <.001). At the end of maintenance, 72% of maintenance rituximab patients reported a CR compared with 52% of patients in the observation arm (P = .0001). Further, 52% of responders in the maintenance rituximab arm converted from a PR to a CR in contrast to 30% of responders in the observation arm (P <.0001).12
The Watch and Wait study is a phase III randomized trial that enrolled 462 patients with asymptomatic, non-bulky stage 2, 3, or 4 FL.46 Patients were randomized either to watchful waiting (observation) or to treatment with rituximab, which was administered in 1 of 2 different schedules. Patients in both treatment groups received rituximab weekly for 4 weeks with 1 of the groups receiving maintenance rituximab once every 2 months for 2 years. Early analysis revealed that the treatment group with maintenance rituximab was superior to the singleagent rituximab arm (no maintenance rituximab), leading to discontinuation of this study arm.46 The median follow-up was 34 months at the time of analysis. The results from follow-up of patients in the 3 original study arms showed that the time to initiation of new therapy was significantly increased by rituximab. At 3 years, 49% of patients in the watchful waiting arm had not received any treatment compared with 80% in the group who received single-agent rituximab and 91% who received rituximab plus maintenance rituximab. Progression-free survival was also significantly improved.46 After 3 years, 30% of patients in the watchful waiting group had not progressed compared with 60% of patients who received rituximab and 81% of patients treated with rituximab plus maintenance rituximab. Further follow-up will reveal if there is an OS difference among the 3 study arms; 96% of the patients are still alive in each group.
A systematic review and meta-analysis of maintenance trials showed that maintenance rituximab improved PFS in both the front-line and relapsed settings and improved OS in patients with relapsed FL who respond to induction therapy.47
Other Lymphomas
Rituximab has shown effectiveness when combined with hyper-CVAD (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) alternating with highdose methotrexate and cytarabine for patients with newly diagnosed mantle cell lymphoma, Burkitt’s lymphoma, and mature B-cell acute lymphoblastic lymphoma.48 The OR rate for patients with mantle cell lymphoma was 97% (CR 87%), and the 5-year failure-free survival and OS rates were 48% and 65%, respectively. Among patients 65 years and younger, the 5-year failure-free survival rate was 60%. For patients with Burkitt’s lymphoma or B-cell acute lymphoblastic lymphoma, the OR rate was 97% (CR 86%). With a median follow-up of 22 months, the estimated 3-year OS, DFS, and EFS rates were 89%, 88%, and 80%, respectively.48 Phase II results have shown rituximab plus bendamustine improved response rates and PFS survival in patients with relapsed, indolent lymphomas or mantle cell lymphoma. Outcomes were similar with indolent or mantle cell histologies.49 Newer drug combinations for patients with Waldenström’s macroglobulinemia (eg, bortezomib, dexamethasone, and rituximab) have produced high response rates (96%), including complete remissions (17%).50
Safety of Rituximab
The safety of rituximab has been evaluated for over a decade, with an estimated total of 1.56 million drug exposures to date (with an average of 6 doses per patient).51 The most common adverse reactions to rituximab (incidence ≥25%) observed in patients with NHL include infusion reactions, the majority of which were mild to moderate (grade 1 and 2) in nature.16,52 Administration of rituximab can result in serious, including fatal, infusion reactions.14,48 Serious cardiopulmonary infusion reactions culminating in death have been reported to occur in approximately 0.04% to 0.07% of patients.53 The incidence of any grade of infusion reaction was highest during the first infusion (77%) and decreased with each subsequent infusion.52 These infusion reactions generally have resolved with slowing or interruption of the infusion and supportive care. Deaths within 24 hours of rituximab infusion have occurred, and approximately 80% of fatal infusion reactions occurred in association with the first infusion.16,52 Patients should be carefully monitored during infusions, and administration should be discontinued and supportive treatment provided for grade 3 or 4 infusion reactions.16,52
Other common grade 3 and 4 events associated with treatment with single-agent rituximab include infections (4%) and hematologic toxicities (lymphopenia 40%, neutropenia 6%, thrombocytopenia 2%, leukopenia 4%, and anemia 3%).16 The rates of these adverse events may increase with chemotherapy-containing regimens.
With increased experience with rituximab, uncommon adverse events also have been recognized. The exact role of rituximab in these situations is unconfirmed, as most patients received other agents or had complicating medical issues. There have been reports of late-onset neutropenia, which is a rare event (post-marketing reporting rate <0.02%) and is defined as neutropenia occurring >4 weeks after the last dose of rituximab.54 This low rate of late-onset neutropenia may reflect increasing use of single-agent rituximab as maintenance therapy and for the treatment of relapsed low-grade B-cell lymphomas. In a retrospective review, patients who received rituximab-containing chemotherapy for CD20-positive B-cell NHL had a higher rate (24.9%) of late-onset neutropenia, which was self-limited and did not result in serious infections.55 Follow-up on 121 DLBCL patients treated with R-CHOP indicated a 13.2% rate of late-onset neutropenia, with a median time to recovery of 69 days (in all but 2 patients) and only 2 episodes of infection reported in 1 patient.56
Tumor lysis syndrome in patients with bulky lymphadenopathy also has been observed (estimated incidence <0.2%) and can be life-threatening; as such, it requires supportive care (eg, hydration, allopurinol, rasburicase) and close laboratory monitoring.57 Hepatitis B reactivation with fulminant hepatitis, hepatic failure, and death has been reported in patients with prior hepatitis B infection who were treated with rituximab.58 In addition, serious viral infections (including cytomegalovirus, herpes simplex virus, parvovirus B19, varicella zoster virus, West Nile virus, and hepatitis C)—either new, reactivated, or exacerbated—have been identified in clinical studies or post-marketing reports.16 The majority of patients received rituximab in combination with chemotherapy or as part of a hematopoietic stem cell transplant. In some cases, the viral infections occurred as late as 1 year following discontinuation of rituximab and have resulted in death.16 Rituximab-treated patients also are at risk for cardiac arrhythmias, renal toxicity, bowel obstruction, and perforation.59 Rare but fatal cases of progressive multifocal leukoencephalopathy following administration of rituximab in HIV-negative patients have been described in the Research on Adverse Drug Events and Reports project.60 A black box warning has been issued by the FDA.16 Rare cases of a syndrome of reversible posterior leukoencephalopathy, a subacute neurological syndrome manifesting with headaches, cortical blindness, and seizures, also have been described.61,62 Several chemotherapy agents have been described in association with the syndrome. A direct relationship of progressive multifocal leukoencephalopathy and reversible posterior leukoencephalopathy with rituximab has not yet been established, as most of these patients have received multiple therapies.
The long-term use of rituximab as maintenance therapy has raised potential concerns regarding additional toxicity burden in patients. Safety results from the PRIMA and SAKK 35/03 study showed that the safety of maintenance rituximab was consistent with the known safety profile of rituximab with no new or unexpected findings.12,63
To date, reports of the patients developing human antichimeric antibodies against rituximab are rare (1.1% [4/356] in 1 study of patients with low-grade FL), and the clinical significance is unknown.16,57 Finally, rituximab induces B-cell depletion, which may compromise the immune system. Reconstitution of a normal B-cell population usually begins after 6 months, and median B-cell levels return to normal by 12 months following completion of therapy; however, it is unclear whether this process is clinically significant.16,64
Cost-Eeffectiveness of Treatment
Given the rapid advancement of targeted therapies for malignancies, it is important to consider and review the cost of therapy and the subsequent value derived. Economic value is defined by the cost-effectiveness ratio, which is derived by taking into account the differences in costs of treatments, side effects, and long-term care divided by the differences in benefits or outcomes between 2 treatment options. The incremental cost-effectiveness ratio (ICER) is expressed as the additional cost per life-year gained or cost per quality-adjusted life-year (QALY) gained. The commonly cited thresholds of cost-effectiveness range from $50,000 to $100,000.65
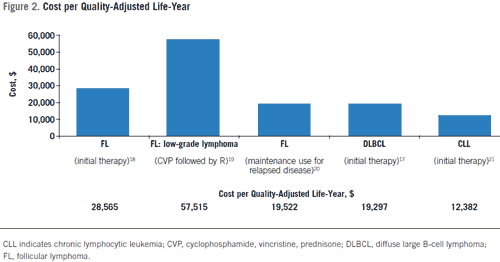
Rituximab has been shown to be consistently costeffective as therapy for FL, DLBCL, and CLL when using commonly cited thresholds (Figure 2).17-21,65 In previously untreated FL, addition of rituximab to CVP is costeffective (ICER $28,565 per QALY), as is maintenance rituximab following 6 to 8 cycles of CVP (ICER $57,515 per QALY).18,19 A recent cost-effectiveness evaluation based on the PRIMA population demonstrated that firstline maintenance rituximab therapy represented greater value for costs than observational practice.66 Based on a United Kingdom National Healthcare Service perspective, the ICER was £15,977 (~$24,958) per QALY gained, well below the assumed willingness to pay threshold of £30,000. The average life expectancy for patients treated with first-line maintenance rituximab was projected to be 1.27 years longer than observed patients and associated with an additional 1.17 QALYs.66 Total costs were £14,129 ($22,069) higher for first-line rituximab maintenance compared with observation and were partially offset by the lower costs of second-line rituximab therapy and supportive care incurred during progression.66
In DLBCL, R-CHOP is estimated to be cost-effective compared with CHOP (ICER of $19,297 per QALY).17 Additional economic analyses of maintenance rituximab for relapsed FL also showed an ICER of $19,522 per QALY.20
An analysis of patients with untreated CLL showed that there were estimated incremental QALYs of 1.82 years with the FCR regimen compared with FC alone.21 Assuming a shorter time horizon of 15 years, FCR would generate an additional 1.41 years in mean life expectancy and 2.04 years of PFS compared with FC chemotherapy. Total direct costs were estimated to be higher for FCR by $22,503 per patient, which was partially offset by reductions in total medication and monitoring costs incurred in the progressed disease state, resulting in an ICER of $12,382 per QALY gained for FCR.21 Indeed, the predominance of available data supports the cost-effectiveness of rituximab in NHL and CLL.17-21
Ongoing Study of Rituximab
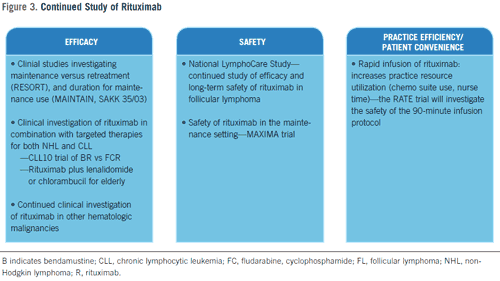
Clinical Investigation of Rituximab
Rituximab continues to undergo vigorous clinical study in a number of B-cell malignancies and disease settings to improve efficacy and safety (Figure 3). In the maintenance setting for the treatment of FL, the ongoing randomized phase III RESORT trial (ECOG 4402) in untreated patients with low tumor burden stage III/IV FL is evaluating single-agent rituximab as initial therapy followed by either maintenance rituximab (a single dose every 3 months) until progression or retreatment with rituximab upon progression.67 This study is designed to determine which strategy leads to the most benefit and delays the time to the development of resistance to rituximab.
The question of optimal duration of maintenance therapy is under investigation in 2 trials. Based on the positive results of the SAKK 35/98 trial, a follow-on study, SAKK 35/03, is investigating the benefit of long-term maintenance rituximab use.63 This trial has enrolled 270 patients (both relapsed and untreated) to receive single-agent rituximab as induction therapy, with responding patients to be randomized to receive maintenance rituximab once every 2 months for 4 treatments or 1 dose every 2 months for 5 years (or until disease progression or undue toxicity).63 In the front-line setting, the randomized phase III study MAINTAIN (NHL-7), with a planned enrollment of 874 patients with advanced low-grade and mantle cell lymphoma, will compare the maintenance schedule of once every 2 months for 2 years to once every 2 months for 4 years.67
Rituximab is being studied in combination with other targeted agents, including lenalidomide, bendamustine, bortezomib, and alemtuzumab, for the treatment of NHL and CLL.67 The BR regimen has been reported to be efficacious in patients with relapsed CLL.68 The German CLL group is conducting a randomized phase III trial (CLL10) comparing the efficacy and safety of FCR and BR regimens in untreated patients with CLL. A small phase II trial is investigating rituximab in combination with lenalidomide in patients with previously treated CLL.69 This study allows for dose reduction of lenalidomide in cases of undue toxicity. Rituximab-containing regimens utilizing targeted therapies, including proteasome and protein inhibitors and antibodies, may permit the omission of chemotherapy agents with their associated toxicities and offer effective treatment options to patients with high unmet needs in the relapsed and salvage settings. Such efficacious and potentially safer treatment regimens could result in reduced ancillary costs from the use of fewer supportive care agents (granulocyte colony-stimulating factor, antiemetics), as demonstrated in the StiL clinical trial. Rituximab also is being investigated as therapy in Hodgkin lymphoma based on the observation that it depletes the few CD20- expressing Hodgkin/Reed-Sternberg cells and thus perhaps kills Hodgkin/Reed-Sternberg stem cells.70,71
Rituximab Use in the Community Practice
Maintenance therapy is used routinely in community practices in the United States and patterns of use of maintenance rituximab have been reported upon by the National LymphoCare Study.72,73 This prospective observational study was designed to collect information on patterns of diagnosis, treatment regimens, and outcomes for patients with newly diagnosed FL in the United States. The study enrolled 2734 patients (83% from community practices) between 2004 and 2007 and represents the entire geography of the country. Initial treatment and maintenance or observation decisions were made by the treating physician. Patients who did not progress within 215 days of completing front-line induction were classified as either receiving maintenance rituximab or observation.73 Of the 1046 patients receiving rituximab-based induction, 220 received single-agent rituximab; 195 R-CVP; 467 R-CHOP, 122 R-fludarabine, and 42 R-other regimen.73 After initial treatment with rituximab monotherapy, 54% of patients received maintenance rituximab and 46% were observed. Following R-chemotherapy, 45% of patients received maintenance rituximab and 55% were observed. Patients on maintenance rituximab were more likely to have FL Grade 1 or 2, stage 3 or 4 disease, normal LDH, involvement of more than 4 lymph nodes, and 2 or more extranodal sites.73 There were no differences in maintenance use by age, gender, race, or FLIPI prognostic score.73
Practical Considerations: Rapid Infusion of Rituximab
Standard administration of rituximab according to the approved schedule can take between 4 and 6 hours to mitigate the risk of infusion-related events (see Safety of Rituximab, above).16,52 The result is a time- and labor-intensive procedure for both practices and patients. Several small studies have demonstrated the safety and feasibility of administering rituximab by rapid infusion, either a 60-minute or 90-minute protocol after standard administration of the first dose.52,74-78 Further, a prospective study of 61 DLBCL patients on the 90-minute protocol reported efficacy comparable to that observed with standard infusion in both the phase III GELA and MInT trials.10,78,79 An ongoing phase III, open-label trial (the RATE study) is investigating the safety of the 90-minute infusion protocol in 385 patients with previously untreated DLBCL or FL.80 Shorter infusion times will yield substantial time savings for patients and benefit outpatient infusion facilities by increasing both the number of infusion chairs available during clinic hours and nursing efficiencies.
Discussion
Rituximab was one of the first drugs to mark the beginning of the new era of molecularly targeted therapy in oncology and was the first approved monoclonal antibody for cancer. Rituximab has changed the treatment paradigms and outcomes for all CD20 NHL and possibly represents the most noteworthy advance in lymphoma treatment over the past decade.81 More recently, large randomized trials have confirmed the significant improvement in PFS for patients with both untreated and relapsed CLL who were treated with a rituximab-containing regimen. Further, for the first time in the treatment of CLL, a significant survival benefit has been demonstrated with FCR therapy in the first-line setting, particularly for Binet stage B and C patients.14 These clinical improvements come with reasonable cost per QALY, and in most FL and all DLBCL and CLL settings studied to date the incremental costs are nominal. By either of the commonly cited dollar value measures (the $100,000 or $50,000 threshold), rituximab is considered cost-effective therapy. Rituximab is used to treat a wide variety of B-cell—derived hematologic malignancies and continues to undergo rigorous clinical investigation in a number of diseases and settings to further improve outcomes and address remaining questions on the optimal use of this biologic therapy.
About the Author
Charles M. Farber, MD, PhD, is an oncologist in the Department of Medicine at the Carol G. Simon Cancer Center/Morristown Memorial Hospital in Morristown, NJ. Randy C. Axelrod, MD, is the Medical Director of Sentara Health System in Norfolk, VA.
Author Affiliations: From the Department of Medicine (CMF), Morristown Memorial Hospital, Carol G. Simon Cancer Center, Morristown, NJ; and Sentara Health System (RCA), Norfolk, VA.
Funding Source: Support for third-party writing assistance for this article was provided by Genentech, Inc.
Disclosures: Dr Farber reports serving as a scientific advisory board member for the National LymphoCare Study and serving on the speakers’ bureau for Genentech. Dr Axelrod reports serving as a consultant for Genentech employer health only and providing expert testimony for Genentech related to other products and the P&T process.
Address correspondence to: Charles M. Farber, MD, PhD, Department of Medicine, Morristown Memorial Hospital, Carol G. Simon Cancer Center, 100 Madison Avenue, Box 1089, Morristown, NJ 07962; or e-mail: charles.farber@atlantichealth.org.
References
1. US Food and Drug Administration. Rituxan label and approval history. http://www.accessdata.fda.gov/Scripts/cder/DrugsatFDA/index.cfm?fuseaction=Search.Label_ApprovalHistory#apphist. Accessed January 16, 2011.
2. Garcia-Sanz R, Orfão A, González M, et al. Primary plasma cell leukemia: clinical, immunophenotypic, DNA ploidy, and cytogenetic characteristics. Blood. 1999;93(3):1032-1037.
3. Srinivas S, Yook C, Chang V, et al. Prevalence of bone marrow CD20 positivity in patients (pts) with multiple myeloma (MM). J Clin Oncol. 2001;20(suppl): abstract 2687.
4. Treon SP, Kelliher A, Keele B, et al. Expression of serother-apy target antigens in Waldenstrom’s macroglobulinemia: therapeutic applications and considerations. Semin Oncol. 2003;30(2):248-252.
5. National Comprehensive Cancer Network (NCCN). NCCN drugs & biologics compendium. http://www.nccn.org/professionals/drug_compendium/ content/contents.asp. Assessed January 16, 2011.
6. Hiddemann W, Kneba M, Dreyling M, et al. Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood. 2005;106(12):3725-3732.
7. Marcus RE, Imrie K, Solal-Celigny P, et al. Phase III study of R-CVP compared with cyclophosphamide, vincristine, and prednisone alone in patients with previously untreated advanced follicular lymphoma. J Clin Oncol. 2008;26(28):4579-4586.
8. Forstpointner R, Dreyling M, Repp R, et al. The addition of rituximab to a combination of fludarabine, cyclophosphamide, mitoxantrone (FCM) significantly increases the response rate and prolongs survival as compared with FCM alone in patients with relapsed and refractory follicular and mantle cell lymphomas: results of a prospective randomized study of the German Low- Grade Lymphoma Study Group. Blood. 2004;104(10):3064-3071.
9. van Oers MH, Klasa R, Marcus RE, et al. Rituximab maintenance improves clinical outcome of relapsed/resistant follicular non-Hodgkin lymphoma, both in patients with and without rituximab during induction: results of a prospective randomized phase III intergroup trial. Blood. 2006;108(10):3295-3301.
10. Pfreundschuh M, Kuhnt E, Trümper L, et al. Randomised intergroup trial of first line treatment for young low-risk patients (<61 years) with diffuse large B-cell non-Hodgkin’s lymphoma (DLBCL) with a CHOP-like regimen with or without the anti-CD20 antibody rituximab—6-year follow-up of the Mint study of the Mabthera international trial (MInT) group [American Society of Hematology annual meeting abstracts]. Blood. 2010;116(21):abstract 111.
11. Coiffier B, Thieblemont C, Van Den Neste E, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood. 2010;116(12):2040-2045.
12. Salles GA, Catalano J, Feugier P, et al. Rituximab maintenance for 2 years in patients with high tumour burden follicular lymphoma responding to rituximab plus chemotherapy (PRIMA): a phase 3, randomised controlled trial. Lancet. 2011;377(9759):42-51.
13. van Oers MH, Van Glabbeke M, Giurgea L, et al. Rituximab maintenance treatment of relapsed/resistant follicular non-Hodgkin’s lymphoma: long-term outcome of the EORTC 20981 phase III randomized intergroup study. J Clin Oncol. 2010;28(17):2853-2858.
14. Hallek M, Fischer K, Fingerle-Rowson G, et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 2010;376(9747):1164-1174.
15. Robak T, Dmoszynska A, Solal-Céligny P, et al. Rituximab plus fludarabine and cyclophosphamide prolongs progression-free survival compared with fludarabine and cyclophosphamide alone in previously treated chronic lymphocytic leukemia. J Clin Oncol. 2010;28(10):1756-1765.
16. Rituxan [package insert]. South San Francisco, CA: Genentech Inc; 2010. http://www.gene.com/gene/products/information/pdf/ rituxan-prescribing.pdf. Accessed January 16, 2011.
17. Hornberger JC, Best JH. Cost utility in the United States of rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone for the treatment of elderly patients with diffuse large B-cell lymphoma. Cancer. 2005;103(8):1644-1651.
18. Hornberger J, Reyes C, Dubeck D, Valente N. Economic evaluation of rituximab plus cyclophosphamide, vincristine and prednisolone for advanced follicular lymphoma. Leuk Lymphoma. 2008;49(2):227-236.
19. Hornberger JC, Reyes C, Shewade A, Loecke D, Valente N. Cost-effectiveness of rituximab post CVP induction for the treatment of low-grade NHL. Blood. 2007;110(11): abstract 4486.
20. Hayslip JW, Simpson KN. Cost-effectiveness of extended adjuvant rituximab for US patients aged 65-70 years with follicular lymphoma in second remission. Clin Lymphoma Myeloma. 2008;8(3):166-170.
21. Carr E, Lerner S, Rick Aultman R, Ute Weisgerber-Kriegl U, Michael Keating M. Treatment effect of first line rituximab, fludarabine and cyclophosphamide in a chronic lymphocytic leukemia patient cohort: an evaluation of prognostic factors, estimated life expectancy and economic outcomes. Blood. 2008;112(11): abstract 2396.
22. Habermann TM, Weller EA, Morrison VA, et al. Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol. 2006;24(19):3121-3137.
23. Winter JN, Weller EA, Horning SJ, et al. Prognostic significance of Bcl-6 protein expression in DLBCL treated with CHOP or R-CHOP: a prospective correlative study [published correction appears in Blood. 2007;109(6):2292]. Blood. 2006;107(11):4207-4213.
24. Gisselbrecht C, Glass B, Mounier N, et al. R-ICE versus R-DHAP in relapsed patients with CD20 diffuse large B-cell lymphoma (DLBCL) followed by autologous stem cell transplantation: CORAL study. J Clin Oncol. 2009;27(suppl): abstract 8509.
25. Kewalramani T, Zelenetz AD, Nimer SD, et al. Rituximab and ICE as second-line therapy before autologous stem cell transplantation for relapsed or primary refractory diffuse large B-cell lymphoma. Blood. 2004;103(10):3684-3688.
26. Haioun C, Mounier N, Emile JF, et al. Rituximab compared to observation after high-dose consolidative first-line chemotherapy (HDC) with autologous stem cell transplantation in poor-risk diffuse large B-cell lymphoma: updated results of the LNH98-B3 GELA study. J Clin Oncol. 2007;25(suppl):abstract 8012.
27. Witzig TE, Geyer SM, Kurtin PJ, et al; North Central Cancer Treatment Group. Salvage chemotherapy with rituximab DHAP for relapsed non-Hodgkin lymphoma: a phase II trial in the North Central Cancer Treatment Group. Leuk Lymphoma. 2008;49(6):1074-1080.
28. Cabanillas F, Liboy I, Rodriguez-Monge E, et al. GROC (gemcitabine, rituximab, oxaliplatin combination) plus pegfilgrastim is less toxic and as active as DHAP and ESHAP for relapsed aggressive non-Hodgkin’s lymphoma (NHL). J Clin Oncol. 2008;26(suppl):abstract 8530.
29. Byrd JC, Peterson BL, Morrison VA, et al. Randomized phase 2 study of fludarabine with concurrent versus sequential treatment with rituximab in symptomatic, untreated patients with B-cell chronic lymphocytic leukemia: results from Cancer and Leukemia Group B 9712 (CALGB 9712). Blood. 2003;101(1):6-14.
30. Byrd JC, Rai K, Peterson BL, et al. Addition of rituximab to fludarabine may prolong progression-free survival and overall survival in patients with previously untreated chronic lymphocytic leukemia: an updated retrospective comparative analysis of CALGB 9712 and CALGB 9011. Blood. 2005;105(1):49-53.
31. Tam CS, O’Brien S, Wierda W, et al. Long-term results of the fludarabine, cyclophosphamide, and rituximab regimen as initial therapy of chronic lymphocytic leukemia. Blood. 2008;112(4):975-980.
32. Wierda W, O’Brien S, Faderl S, et al. A retrospective comparison of three sequential groups of patients with recurrent/refractory chronic lymphocytic leukemia treated with fludarabine-based regimens. Cancer. 2006;106(2):337-345.
33. Wierda W, O’Brien S, Wen S, et al. Chemoimmunotherapy with fludarabine, cyclophosphamide, and rituximab for relapsed and refractory chronic lymphocytic leukemia. J Clin Oncol. 2005;23(18):4070-4078.
34. Stilgenbauer S, Zenz T, Winkler D, et al. Genomic aberrations, VH mutation status and outcome after fludarabine and cyclophosphamide (FC) or FC plus rituximab (FCR) in the CLL8 Trial [American Society of Hematology annual meeting abstracts]. Blood. 2008;112: abstract 781.
35. Li J, Zhi J, Wenger MK, et al. Higher doses of rituximab may be required for patients with CLL as compared to NHL based on population pharmacokinetic (PK) modeling [American Society of Hematology annual meeting abstracts]. Blood. 2009;114: abstract 1742.
36. Cheson BD, Gregory SA, Marcus R. Emerging treatments for indolent lymphoma. Clin Adv Hematol Oncol. 2007;5(5 suppl 8):1-9.
37. Salles G, Mounier N, de Guibert S, et al. Rituximab combined with chemotherapy and interferon in follicular lymphoma patients: results of the GELA-GOELAMS FL2000 study. Blood. 2008;112(13):4824-4831.
38. Herold M, Haas A, Srock S, et al; East German Study Group Hematology and Oncology Study. Rituximab added to first-line mitoxantrone, chlorambucil, and prednisolone chemotherapy followed by interferon maintenance prolongs survival in patients with advanced follicular lymphoma: an East German Study Group Hematology and Oncology Study. J Clin Oncol. 2007;25(15):1986-1992.
39. Rummel MJ, Niederle N, Maschmeyer G, et al. Bendamustine plus rituximab is superior in respect of progression free survival and CR rate when compared to CHOP plus rituximab as first-line treatment of patients with advanced follicular, indolent, and mantle cell lymphomas: final results of a randomized phase III study of the StiL (Study Group Indolent Lymphomas, Germany) [American Society of Hematology annual meeting abstracts]. Blood. 2009;114:abstract 405.
40. van Oers MH. Rituximab maintenance therapy: a step forward in follicular lymphoma. Haematologica. 2007;92(6):826-833.
41. Hochster HS, Weller E, Gascoyne RD, et al. Maintenance rituximab after cyclophosphamide, vincristine, and prednisone prolongs progression- free survival in advanced indolent lymphoma: results of the randomized phase III ECOG1496 Study. J Clin Oncol. 2009;27(10):1607-1614.
42. Martinelli G, Schmitz SF, Utiger U, et al. Long-term follow-up of patients with follicular lymphoma receiving single-agent rituximab at two different schedules in trial SAKK 35/98. J Clin Oncol. 2010;28(29):4480-4484.
43. Hainsworth JD, Litchy S, Shaffer DW, Lackey VL, Grimaldi M, Greco FA. Maximizing therapeutic benefit of rituximab: maintenance therapy versus re-treatment at progression in patients with indolent non Hodgkin’s lymphoma—a randomized phase II trial of the Minnie Pearl Cancer Research Network. J Clin Oncol. 2005;23(6):1088-1095.
44. Forstpointner R, Unterhalt M, Dreyling M, et al; German Low Grade Lymphoma Study Group (GLSG). Maintenance therapy with rituximab leads to a significant prolongation of response duration after salvage therapy with a combination of rituximab, fludarabine, cyclophosphamide and mitoxantrone (R-FCM) in patients with relapsed and refractory follicular and mantle cell lymphomas—results of a prospective randomized study of the German Low Grade Lymphoma Study Group (GLSG). Blood. 2006;108(13):4003-4008.
45. Foá R, Di Rocco A, van Hazel G, et al. Maintenance rituximab every 2 months for 2 years is effective and well tolerated in patients with follicular lymphoma with both standard or rapid infusion: updated results from the phase IIIb MAXIMA study [American Society of Hematology annual meeting abstracts]. Blood. 2010;116(21):abstract 3945.
46. Ardeshna KM, Smith P, Qian W, et al. An Intergroup randomised trial of rituximab versus a watch and wait strategy in patients with stage II, III, IV, asymptomatic, non-bulky follicular lymphoma (grades 1, 2 and 3a). A preliminary analysis [American Society of Hematology annual meeting abstracts]. Blood. 2010;116(21):abstract 6.
47. Vidal L, Gafter-Gvili A, Salles G, et al. Rituximab maintenance for the treatment of patients with follicular lymphoma: systematic review and meta-analysis of randomized trials—2010 update. [American Society of Hematology annual meeting abstracts]. Blood. 2010;116(21):abstract 1798.
48. Fayad L, Thomas D, Romaguera J. Update of the M. D. Anderson Cancer Center experience with hyper-CVAD and rituximab for the treatment of mantle cell and Burkitt-type lymphomas. Clin Lymphoma Myeloma. 2007;8(suppl 2):S57-S62.
49. Robinson KS, Williams ME, van der Jagt RH, et al. Phase II multicenter study of bendamustine plus rituximab in patients with relapsed indolent B-cell and mantle cell non-Hodgkin’s lymphoma. J Clin Oncol. 2008;26(27):4473-4479.
50. Treon SP, Ioakimidis L, Soumerai JD, et al. Primary therapy of Waldenstrom’s macroglobulinemia with bortezomib, dexamethasone, and rituximab: results of WMCTG clinical trial 05-180. J Clin Oncol. 2008;26(suppl):abstract 8519.
51. Richey EA, Carson KR, Evens AM, et al. “Beating the bushes” to identify previously unreported cases of a rare and potentially fatal adverse drug reaction: comparison of HIV-negative rituximab-associated progressive multifocal leucoencephalopathy (PML) cases obtained by the Research on Adverse Drug Events and Report (RADAR), the FDA, the manufacturer, and a literature review. J Clin Oncol. 2009;27:7(suppl 7): abstract 6604.
52. Sehn LH, Donaldson J, Filewich A, et al. Rapid infusion rituximab in combination with corticosteroid-containing chemotherapy or as maintenance therapy is well tolerated and can safely be delivered in the community setting. Blood. 2007;109(10):4171-4173.
53. Kunkel L, Wong A, Maneatis T, et al. Optimizing the use of rituximab for treatment of B-cell non-Hodgkin’s lymphoma: a benefit-risk update. Semin Oncol. 2000;27(6 suppl 12):53-61.
54. Benyunes MC, Multani PS, Saunders A. Neutropenia in patients treated with rituximab. N Engl J Med. 2003;348(26):2691-2694.
55. Nitta E, Izutsu K, Sato T. A high incidence of late-onset neutropenia following rituximab-containing chemotherapy as a primary treatment of CD20-positive B-cell lymphoma: a single-institution study. Ann Oncol. 2007;18(2):364-369.
56. Lai GG, Lim ST, Tao M, Chan A, Li H, Quek R. Late-onset neutropenia following RCHOP chemotherapy in diffuse large B-cell lymphoma. Am J Hematol. 2009;84(7):414-417.
57. Kimby E. Tolerability and safety of rituximab (MabThera). Cancer Treat Rev. 2005;31(6):456-473.
58. Aksoy S, Harputluoglu H, Kilickap S, et al. Rituximab-related viral infections in lymphoma patients. Leuk Lymphoma. 2007;48;1307-1312.
59. Maloney DG, Grillo-López AJ, White CA, et al. IDEC-C2B8 (Rituximab) anti-CD20 monoclonal antibody therapy in patients with relapsed lowgrade non-Hodgkin’s lymphoma. Blood. 1997;90(6):2188-2195.
60. Carson KR, Evens AM, Richey EA, et al. Progressive multifocal leukoencephalopathy following rituximab therapy in HIV negative patients: a report of 57 cases from the Research on Adverse Drug Event and Reports project. Blood. 2009;113(20):4834-4840.
61. Haefner M, Siciliano R, Widmer L, Vogel Wigger BM, Frick S. Reversible posterior leukoencephalopathy after treatment of diffuse large B cell lymphoma. Onkologie. 2007;30(3):138-140.
62. Vaughn C, Zhang L, Schiff D. Reversible posterior leukoencephalopathy in cancer. Curr Oncol Rep. 2008;10(1):86-91.
63. Taverna CJ, Bassi S, Hitz F, et al. Rituximab maintenance treatment for a maximum of 5 years in follicular lymphoma: safety analysis of the randomized phase III trial SAKK 35/03 [American Society of Hematology annual meeting abstracts]. Blood. 2010;116(21):abstract 1802.
64. Ram R, Ben-Bassat I, Shpilberg O, Polliack A, Raanani P. The late adverse events of rituximab therapy—rare but there! Leuk Lymphoma. 2009;50(7):1083-1095.
65. Lee CP, Chertow GM, Zenios SA. An empiric estimate of the value of life: updating the renal dialysis cost-effectiveness standard. Value Health. 2009;12(1):80-87.
66. Papadakis K, Follows G, Boyer J, et al. Cost effectiveness analysis of rituximab maintenance in patients with untreated high tumour burden follicular lymphoma after response to immunochemotherapy: a UK National Healthcare Services perspective [American Society of Hematology annual meeting abstracts]. Blood. 2010;116(21):abstract 3833.
67. National Institutes of Health. ClinicalTrials.gov. Rituximab clinical trials. http://www.clinicaltrials.gov/ct2/results?term=rituximab. Accessed January 13, 2009.
68. Fischer K, Stilgenbauer S, Schweighofer CD, et al. Bendamustine in combination with rituximab (BR) for patients with relapsed chronic lymphocytic leukemia (CLL): a multicentre phase II trial of the German CLL Study Group (GCLLSG) [American Society of Hematology annual meeting abstracts]. Blood. 2008;112:abstract 330.
69. Ferrajoli A, Badoux XC, O’Brien S, et al. Combination therapy with lenalidomide and rituximab in patients with relapsed chronic lymphocytic leukemia (CLL) [American Society of Hematology annual meeting abstracts]. Blood. 2009;114:abstract 206.
70. Jones RJ, Gocke CD, Kasamon YL, et al. Circulating clonotype B cells in classic Hodgkin lymphoma. Blood. 2009;113(23):5920-5926.
71. Younes A, Romaguera J, Hagemeister F, et al. A pilot study of rituximab in patients with recurrent, classic Hodgkin disease. Cancer. 2003;98(2):310-314.
72. Friedberg JW, Taylor MD, Cerhan JR, et al. Follicular lymphoma in the United States: first report of the National LymphoCare Study. J Clin Oncol. 2009;27(8):1202-1208.
73. Flowers C, Taylor M, Hirata J, et al. Use of maintenance rituximab (R) in the United States following R-based induction for follicular lymphoma (FL). J Clin Oncol. 2010;28(suppl 15s):abstract 8100.
74. Provencio M, Cerdeira S, Bonilla F, Sánchez A, España P. Rapid-infusion rituximab in lymphoma treatment. Ann Oncol. 2006;17(6):1027-1028.
75. Siano M, Lerch E, Zucca E, Mora O, Sessa C, Ghielmini M. A phase I-II study to determine the maximum tolerated infusion-rate of rituximab, with a special emphasis on monitoring the effect of rituximab on cardiac function. Clin CancerRes. 2008;14(23):7935-7939.
76. Salar A, Casao D, Cervera M, et al. Rapid infusion of rituximab with or without steroid-containing chemotherapy: 1-yr experience in a single institution. Eur J Haematol. 2006;77(4):338-340.
77. Corey P, Go R, Schaper A. A nurse can safely deliver rituximab over 90 minutes. Oncology Nursing Society 32nd Annual Congress; April 24-27, 2007; Las Vegas, NV. Abstract 2010.
78. Gibbs S, Pout G, Wimperis J. Rapid infusion rituximab is as clinically effective and safe as conventional infusion regimes in the treatment of diffuse large B-cell lymphoma: a 2-year prospective study. Haematologica. 2007;92(suppl 2):abstract 0708.
79. Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002;346(4):235-242.
80. National Institutes of Health. ClinicalTrials.gov. A study of rituximab alternative dosing rate in patients with previously untreated diffuse large B-cell or follicular non-Hodgkin’s lymphoma (RATE). http://www.clinicaltrials.gov/ct2/ show/NCT00719472?term=RATE&rank=4. Accessed January 16, 2011.
81. Horning SJ. Follicular lymphoma, survival, and rituximab: is it time to declare victory? J Clin Oncol. 2008;26(28):4537-4538. 82. Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtypes in the United States, 1992=2001. Blood. 2006;107(1):265-276.










