Publication
Article
Contemporary Oncology®
The Use of Tyrosine Kinase Inhibitors for Gastrointestinal Stromal Tumors (GIST)
Author(s):
In this review article, the author discusses the use of tyrosine kinase inhibitors in the management of patients with gastrointestinal stromal tumors.
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors of the gastrointestinal tract, with an annual incidence of 12 to 14 per million persons.1 The tumors are found in the stomach (52%), small intestine (25%), colon (11%), esophagus (5%), and rectum (2%), as well as in the omentum, mesentery, and peritoneum.2 The cellular origin of GISTs is thought to be the interstitial cells of Cajal (ICC), the intestinal pacemaker.3 GISTs appear histologically similar to leiomyosarcomas of the GI tract but are positive for the immunohistochemical marker for the KIT protein (CD117).4 The tumors occur in three histologic variants: spindle cell type (70%), epithelial type (20%), and combined spindle cell-epithelial type (10%).
The characteristic pathologic feature of GISTs is the activating mutations of KIT, which occur in roughly 85% of cases.5 Approximately 5% to 8% of GISTs have mutations of the platelet-derived growth factor receptor alfa (PDGFRα) gene6 and wild-type GIST accounts for the remainder of GIST mutations. The most common KIT mutation is on exon 11 (64%), followed by exon 9 (15%), exon 13 (<2%), and exon 17 (1%).7 The most common PDGFRα mutation is the D842V substitution on exon 18.8 The majority of exon 9 mutations occur in the small bowel and most PDGFRα mutations occur in the stomach. The exon 11 mutations are distributed throughout the GI tract.
The presenting signs and symptoms of GIST vary from abdominal pain, bloating, or bleeding, to incidental findings on imaging or at the time of surgery. Surgery is the mainstay of treatment for localized GIST. Clinical prognostic variables used to predict recurrence include tumor size, mitotic activity, and location of the tumor within the GI tract; high-risk factors include size >5 cm, >5 mitoses per 50 high-power fields, and location in the small bowel.9,10 The use of exon mutational analyses as an independent risk factor is under investigation.
TKIs for Metastatic GIST
Imatinib
Patients with metastatic or surgically nonresectable disease do not respond to the standard cytotoxic therapy used for sarcomas, and have poor outcomes. With the introduction of imatinib (Gleevec), an oral tyrosine kinase inhibitor (TKI) that selectively targets KIT, ABL, BCR-ABL, and PDGFR, up to 80% of patients experience clinical benefit, with stable or responding disease lasting a median of approximately 20 months.11-14 Common side effects of imatinib include fluid retention, rash, arthralgias, myalgias, nausea, and fatigue.
Two large phase III trials compared once-daily imatinib 400 mg to a twice-daily 400 mg regimen in patients with metastatic GIST. These two studies—conducted in the United States and Canada by the Southwest Oncology Group (SWOG)12 and in Europe and Australia (EU-AUS) by the European Organization for Research and Treatment of Cancer, the Italian Sarcoma Group, and the Australasian Gastro-Intestinal Trials Group14—used the same selection criteria for study entry, treatment, and follow-up, the purpose being to later combine data. A total of 743 patients were enrolled in the SWOG trial and were followed for a median of 54 months. The median progression-free survival (PFS) was 18 months on once-daily imatinib and 20 months on the twice-daily imatinib, with median overall survival (OS) of 55 months and 51 months, respectively. There was no statistically significant difference in response rates, PFS, or OS between the two dosages. The EU-AUS enrolled 946 patients and their initial report, with a median follow up of slightly over 25 months, demonstrated a PFS advantage for the twice-daily dosing but no OS advantage. Subsequently, with longer follow up of 40 months, the EU-AUS investigators reported that once-daily and twice-daily dosing resulted in similar PFS and OS.15
Combining the SWOG and EU-AUS data with those from a median follow-up of 45 months, a meta-analysis of 1640 patients showed a small but significant PFS-related difference in patients on the twice-daily regimen as compared to those treated with the standard single dose (estimated hazard ratio [HR], 0.89; 95% CI, 0.79-1.00 but significant [P = .04, Wald test]). The benefit of the higher dose of imatinib was seen mainly in patients with the KIT exon 9 mutation.16 The OS was identical in both arms.
What then should be the initial dose of imatinib for patients with metastatic GIST? Should patients with the exon 9 mutation be started at a higher dose? Because overall survival is similar with both dosages and because higher doses of imatinib are associated with increased toxicity, it is reasonable to start all patients with metastatic GIST on 400 mg per day. If a tumor has an established exon 9 mutation, and response to therapy is important, an initial higher dose of imatinib should be used.
Specific treatment options show promise for the rare exon 18 mutation in PDGFRα, D842V, and wildtype GIST, which are more resistant to imatinib.17 Masitinib, for example, is a new TKI with greater in vitro activity and selectivity for the wild-type c-KIT receptor than imatinib. When masitinib was studied in 30 patients with newly diagnosed metastatic GIST, investigators reported a median PFS of 41.3 months and a 3-year OS of 89.9%.18 Side effects included asthenia, diarrhea, edema, nausea, vomiting, and rash. While the study was small, these findings compare favorably to those seen with imatinib. Further study is warranted to evaluate the effects of masitinib for the wild-type subset. In advanced disease, patients with wild-type GIST might benefit from the combination of TKI and cytotoxic chemotherapy.
Second-Line TKIs
For patients whose disease progresses on the standard once-daily 400 mg dose of imatinib, dosing can be increased to 600 mg or 800 mg per day. The median PFS in the SWOG study on crossover to an 800 mg/day dose was 5 months (95% CI, 2-10 months), with a response rate of 3% (95% CI, 1%-7%).12 In the EU-AUS, the response rate was 2%, with a median PFS of 81 days when switching to the 800 mg/day dose.19
After disease progression or intolerance to imatinib at any dose, the next-line FDA-approved agent is sunitinib (Sutent), an oral multi-targeted receptor TKI of KIT, PDGFR, VEGFR-1, VEGFR-2, VEGFR- 3, FLT3, and RET. In the initial study confirming activity of sunitinib, patients with GIST whose disease progressed or who were unable to tolerate imatinib were randomized to sunitinib 50 mg/day (4 weeks on followed by 2 weeks off) or placebo; 312 patients were randomized in a 2:1 ratio.20 The trial was unblinded at the first interim analysis because of the significantly longer time to tumor progression (TTP) in the sunitinib arm (median TTP, 27.3 weeks [95% CI, 16-32] in the sunitinib group vs 6.4 weeks [95% CI, 4.4-10] in those receiving placebo), at which point patients on placebo could cross over to sunitinib. Attempts to modify the 50 mg/day (4 weeks on, 2 weeks off) regimen to a continuous 37.5 mg/day schedule has been shown to be well tolerated and to have similar efficacy.21 The main adverse effects of sunitinib include fatigue, diarrhea, skin darkening, and nausea.
Other TKIs used in cases of imatinib and sunitinib failure include nilotinib (Tasigna) and sorafenib (Nexavar). Nilotinib is a second-generation TKI with activity against KIT, PDGFR, and BCR-ABL. Despite having similar targets to those of imatinib, nilotinib’s intracellular concentration is 7 to 10 times higher than that of imatinib.22 Nilotinib has clinical activity in patients whose disease has progressed on imatinib or sunitinib, demonstrating a PFS of 12 weeks and a median OS of 34 week.23,24 Clinically important adverse effects are mild, with grade I to II rash, headache, pruritus, fatigue, diarrhea, nausea, and cytopenias.
Sorafenib is a multitargeted inhibitor of RAF/MEK/ERK, KIT, VEGFR, and PDGFR, with clinical activity in third- and fourth-line therapy. Sorafenib has demonstrated in vitro potency against GIST tumors with imatinib-resistant secondary mutations involving the KIT activation loop.25,26 Adverse effects included skin tenderness, hypertension, hypophosphatemia, headache, and fatigue.
Combination Therapy
There is scientific rationale to combine TKIs as they have different pathways of resistance; indeed, combining TKIs may render it possible to overcome resistance. In an open-label, phase I dose-escalation study, patients with imatinib-resistant GIST were treated with nilotinib in combination with imatinb with promising results.23 An ongoing, randomized phase II study of nilotinib alone versus nilotinib combined with imatinib in patients whose disease has progressed on a high dose of imatinib should help delineate the role of combination therapy.
Although standard chemotherapy is not effective against GIST, the combination of imatinib and low-dose doxorubicin has shown activity in imatinib-resistant GIST, especially in wild-type GIST.27 In a phase I/II study, 26 patients with imatinib-resistant GIST were treated with imatinib 400 mg/day and doxorubicin 15-20 mg/m2/weekly x 4 cycles.27 The median overall PFS was 3.3 months (95% CI, 2.1-4.6), but subsequent analysis based on wild-type status revealed a median PFS of 7 months (95% CI, 1.7-12.3) for patients with wild-type GIST and 2.7 months (95% CI, 1.7-3.7; P = .134) for those without (10 mutant, 6 not assessed).
Pointing to other potential targets, a preclinical study demonstrated a 58% reduction in tumor volume with the HSP90 inhibitor IPI-504 combined with imatinib.28 A clinical trial of IPI-504 was terminated early due to severe toxicity. A phase III trial (S0502) comparing imatinib alone to imatinib with bevacizumab was closed early due to poor patient accrual. More recently, insulin-like growth factor receptor inhibitors have been shown to be overexpressed in pediatric GIST and in wild-type GIST, and might be a target in that subset of GIST.29-31 Moreover, the downstream pathways of KIT/PDGFRα, including PI3K, AKT, mTOR, and BRAF, could be targeted in conjunction with imatinib.
Radiographic Response and Progression
Following tumor response in GIST patients treated with imatinib has provided oncologists who specialize in sarcomas with opportunities to explore new endpoints for response. The use of positron emission tomography (PET) [18F] fluorodeoxyglucose (FDG) has been studied extensively in patients with GIST. Patients with advanced GIST who are treated with imatinib and followed by PETFDG will show decreased PET-FDG uptake (decreased SUVmax) within 24 to 48 hours.32-34 Studies have suggested that patients with early responses to imatinib demonstrated by PET-FDG have a significantly better PFS, and that this type of imaging will predict those who will respond to imatinib.32-34 The optimal cut-off of SUVmax and time to obtain PET-FDG is unknown, but a decrease in SUVmax at 2 months is reasonable. It should be noted that Medicare does not cover PET imaging for GIST.
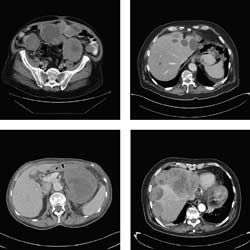
When computed tomography (CT) is used to follow imatinib-treated GISTs, responding tumors will demonstrate decreased density as measured by CT attenuation coefficient (Hounsfield unit [HU]). Paradoxically, such tumors might also show an increase in size, which is thought to reflect central necrosis and swelling of the tumor. Following GIST tumors by size alone is, therefore, inadequate. Choi and colleagues, from the MD Anderson Cancer Center, proposed a new CT criteria for assessing tumor response of GIST that includes not only size, but also incorporates tumor density changes by HU. To this end, a partial response (PR) would be defined as a decrease in size of >10% or a decrease in tumor density of HU >15% with no new lesions and progression would be defined as an increase in tumor size of >10% with failure to meet PR criteria by tumor density (HU) on CT. The remaining findings would be classified as new lesions, new intratumoral nodules, or increase in the size of the existing intratumoral nodules.35 Confirmation and validation of the Choi criteria is now underway by other research groups. The use of Choi criteria for non-GIST tumors has not been validated and RECIST is still used for non-GIST disease.
Interruption of Imatinib Therapy
Patients with advanced GIST are generally continued on imatinib therapy indefinitely as long as they are tolerating therapy and their disease is controlled. There are, however, some patients who have been on imatinib for some period of time and want to discontinue and then resume the treatment when their tumor begins to grow. This is analogous to intermittent androgen blockade for men with metastatic hormone-sensitive prostate cancer. A clinical study by the French sarcoma group tested the hypothesis of interruption of imatinib therapy in responding patients in the BFR14 study.36 Patients on imatinib with responding GISTs were randomized to discontinue treatment at 1 and 3 years or to continue on therapy. Those who discontinued therapy had a median PFS of 6 months and the investigators reported no OS difference between the continuous and the interrupted arms. The concern is that interrupted imatinib therapy might decrease the time to imatinib resistance. The time to imatinib resistance was similar in both arms of the study, but it was under-powered to identify a statistically significant difference.37 The recommendations are to continue imatinib long-term until disease progression or the development of untoward adverse effects,38 but periodic interruptions in imatinib therapy could be considered for selected patients who have toxicities from therapy and understand the risks and benefits of interruption of therapy.
Surgery for Metastatic Disease
Surgery for metastatic GIST is a valid option at initial presentation and for selected patients whose disease progresses on imatinib. Typically, patients with widespread progressive disease while on imatinib or other agents do not benefit from palliative surgery39; however, if a patient on imatinib has isolated disease progression of one or two lesions or within a lesion (intratumoral progression), surgical resection can be beneficial.40,41 The theory is that the other sites of metastatic disease are being controlled with imatinib, but isolated tumor resistance can occur in 1 or 2 of the lesions, and removing the resistant clone can allow patients to continue on imatinib while their other sites of GIST remain under control. The use of ablative options should also be considered. Ablative techniques such as cryoablation and radiofrequency ablation in selected tumor progressions can be performed safely and repeatedly.
Adjuvant Imatinib for Resected GIST
Despite surgical resection of primary disease, some patients will develop recurrent disease. With the efficacy of imatinib in advanced disease, it is postulated that adjuvant therapy with imatinib would improve recurrence-free survival (RFS) and overall survival. Beginning in 2002, a randomized, phase III, double-blind, placebo-controlled trial of imatinib in resected GIST was performed in the United States and Canada (American College of Surgeons Oncology Group [ACOSOG] Z9001).42 Patients with tumors that were both >3 cm in size and KIT-positive were randomly assigned to 1 year of once-daily imatinib (400 mg) or placebo. The primary endpoint of the published study was RFS. The study was terminated early because the pre-determined RFS efficacy boundary was crossed. Of the 718 patients randomized at early termination (median follow-up, 19.7 months), 30 (8%) patients in the imatinib group and 70 (20%) in the placebo group had tumor recurrence, with the use of imatinib significantly improving RFS, as compared to placebo (98% [95% CI, 96-100] vs 83% [78-88]) at 1 year. There was no difference in OS between the groups. Subset analysis post hoc showed recurrencefree benefits in the imatinib group in all tumors based on size >3 cm and <6 cm, >6 cm and <10 cm, and >10 cm, but the major benefit was seen in the >10 cm group.42 Reviewing the recurrence-free curves, it appears that the recurrence-free benefit lasts an additional 6 months after discontinuing imatinib; hence, after 18 months from randomization, the rate of recurrence increases. This 6-month PFS is consistent with the French BFR14 metastatic GIST study, showing a 6-month PFS after discontinuation of imatinib in patients with responsive disease.36
Duration of Therapy
Optimal duration of adjuvant imatinib therapy is being evaluated in 2 studies in Europe. The EORTC is comparing 0 versus 2 years of imatinib and the Scandanavian Sarcoma group (SSG) trial XVIII is comparing 1 versus 3 years of imatinib. The endpoint of both studies is RFS and results will not be available for several years.
The dose of imatinib for these adjuvant trials is 400 mg/day. Increasing the dose to 400 mg twice daily for exon 9 mutations makes theoretical sense and could be considered, but it is unknown if the higher dose of imatinib in this group is beneficial. In addition, none of the reported studies or trials in progress will be able to confirm if adjuvant imatinib will improve OS in high-risk disease. The most we will be able to confirm is the RFS achieved with imatinib.
The ACOSOG Z9001 study did not stratify based on exon mutational analysis nor mitotic activity, but subsequent analysis of Z9001 findings incorporating exon mutational analysis and mitotic activity has been reported.43 Tumor mitotic rate, size, location, and mutation status were available in 513 of 718 patients. On multivariate analysis of the placebo arm, RFS was worse with high mitotic rate, tumor size, small bowel location, and KIT exon 11 mutation. On multivariate analysis in the imatinib arm, RFS was worse with high mitotic rate, tumor size, and small bowel or rectal location. Patients with the KIT exon 9 mutation had similar RFS. There was no statistical difference in RFS between study arms in patients with wild-type KIT and those with PDGFRα.
Are there high-risk groups for which prolonged adjuvant imatinib is justified? Based on the available data, patients with large tumors, especially those >10 cm, and tumors with high mitotic rates of >5 mitoses per 50 high power fields [HPF] are at exceptionally high risk of relapse after discontinuation of imatinib, and could be offered prolonged imatinib therapy (for >1 year). The optimal duration of prolonged therapy is unknown and will need to be reviewed in the context of available data and tolerance to therapy, as the use of adjuvant imatinib may only delay recurrence and might have no impact on OS.
Active Phase III Trials for First-Line Therapy
Currently, there are two major trials in the United States that are open and accruing patients with metastatic GIST for first-line therapy. The first of these trials is sponsored by AB Science (AB1010) and is comparing mastinib to imatinib at 400 mg or 600 mg/day. The other major trial, sponsored by Novartis, is comparing nilotinib to imiatinib. Details on these studies are available at www. clinicaltrials.gov.
CONCLUSION
The treatment of GIST has changed dramatically in the past decade. Prior to the use of imatinib, which has prolonged survival, patients with advanced/metastatic disease had a dismal prognosis. After progression on standard dose of imatinib, additional benefit can be anticipated with increased doses. Although higher doses of imatinib, sunitinib, nilotinib, sorafenib, and other agents have clinical benefit, these benefits are short-lived and newer agents are desperately needed. The use of imatinib after curative surgery can prolong RFS and there is hope that a longer duration of adjuvant therapy might improve outcomes. A greater understanding of exon mutations will be useful in helping to direct and tailor therapies in patients with GIST.
ABOUT THE AUTHOR
Affiliation: Scott H. Okuno, MD, is an associate professor of oncology in the Department of Oncology, Mayo Clinic, in Rochester, Minnesota.
Disclosures: The author reports no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Address correspondence to: Scott H. Okuno, MD, Department of Oncology, Mayo Clinic, 200 First St, SW, Rochester, MN 55905, or e-mail okuno.scott@mayo.edu.
REFERENCES
1. Nilsson B, Bümming P, Meis-Kindblom JM, et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era—a population-based study in western Sweden. Cancer. 2005;103(4):821-829.
2. Corless CL, Fletcher JA, Heinrich MC. Biology of gastrointestinal stromal tumors. J Clin Oncol. 2004;22(18):3813-3825.
3. Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastro-intestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Path. 1998;152(5):1259-1269.
4. Fletcher CDM, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Path. 2002;33(5):459-465.
5. Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279(5350):577-580.
6. Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299(5607):708-710.
7. Debiec-Rychter M, Sciot R, Le Cesne A, et al. KIT mutations and dose selection for imatinib in patients with advanced gastrointestinal stromal tumours. Eur J Cancer. 2006;42(8):1093-1103.
8. Heinrich MC, Corless CL, Demetri GD, et al. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21(23):4342-4349.
9. Dematteo RP, Gold JS, Saran L, et al. Tumor mitotic rate, size, and location independently predict recurrence after resection of primary gastrointestinal stromal tumor (GIST). Cancer. 2008;112(3):608-615.
10. Singer S, Rubin BP, Lux ML, et al. Prognostic value of KIT mutation type, mitotic activity, and histologic subtype in gastrointestinal stromal tumors. J Clin Oncol. 2002;20(18):3898-3905.
11. Demetri, GD, Rubin BP, Lux ML, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347(7):472-480.
12. Blanke CD, Rankin C, Demetri GD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008.26(4):626-632.
13. Blanke CD, Demetri GD, von Mehren M, et al. Long-term results from a randomized phase II trial of standard- versus higherdose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008;26(4):620-625.
14. Verweij J, Casali PG, Zalcberg J, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomised trial. Lancet. 2004;364(9440):1127-1134.
15. Casali P, Verweij J, Kotasek D, et al. Imatinib mesylate in advanced Gastrointestinal Stromal Tumors (GIST): survival analysis of the EORTC ISG AGITG randomized trial in 946 patients [abstract 711]. Eur J Cancer Suppl. 2005;2:201.
16. Gastrointestinal Stromal Tumor Meta-Analysis Group (MetaGIST). Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1640 patients. J Clin Oncol. 28(7):1247-1253.
17. Murray M, Hatcher H, Jessop F, et al. Treatment of wild-type gastrointestinal stromal tumor (WT-GIST) with imatinib and sunitinib. Pediatr Blood Cancer. 2008;50(2):386-388.
18. Le Cesne A, Blay JY, Bui BN, et al. Phase II study of oral masitinib mesilate in imatinib-naive patients with locally advanced or metastatic gastro-intestinal stromal tumour (GIST). Eur J Cancer. 2101;46(8):1344-1351.
19. Zalcberg JR, Verweij J, Casali PG, et al. Outcome of patients with advanced gastro-intestinal stromal tumours crossing over to a daily imatinib dose of 800 mg after progression on 400 mg. Eur J Cancer. 2005;41(12):1751-1757.
20. Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointest-inal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368(9544):1329-1338.
21. George S, Blay JY, Casali PG, et al. Clinical evaluation of continuous daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib failure. Eur J Cancer. 2009;45(11):1959-1968.
22. Prenen H, Guetens G, de Boeck G, et al. Cellular uptake of the tyrosine kinase inhibitors imatinib and AMN107 in gastrointestinal stromal tumor cell lines. Pharmacology. 2006;77(1):11-16.
23. Demetri GD, Casali PG, Blay JY, et al. A phase I study of single-agent nilotinib or in combination with imatinib in patients with imatinib-resistant gastrointestinal stromal tumors. Clin Cancer Res. 2009;15(18):5910-5916.
24. Montemurro M, Schöffski P, Reichardt P, et al. Nilotinib in the treatment of advanced gastrointestinal stromal tumours resistant to both imatinib and sunitinib. Eur J Cancer. 2009;45(13):2293-2297.
25. Huynh H, Lee JW, Chow PK, et al. Sorafenib induces growth suppression in mouse models of gastrointestinal stromal tumor. Mol Cancer Ther. 2009;8(1):152-159.
26. Guo T, Agaram NP, Wong GC, et al. Sorafenib inhibits the imatinib-resistant KITT670I gatekeeper mutation in gastrointestinal stromal tumor. Clin Cancer Res. 2007;13(16):4874-4881.
27. Maurel J, Martins AS, Poveda A, et al. Imatinib plus low-dose doxorubicin in patients with advanced gastrointestinal stromal tumors refractory to high-dose imatinib: a phase I-II study by the Spanish Group for Research on Sarcomas. Cancer. 2010;116(15):3692-3701.
28. Dewaele B, Wasag B, Cools J, et al. Activity of dasati-nib, a dual SRC/ABL kinase inhibitor, and IPI-504, a heat shock protein 90 inhibitor, against gastrointestinal stromal tumor-associated PDGFRAD842V mutation. Clin Cancer Res. 2008;14(18):5749-5758.
29. Agaram NP, Laquaglia MP, Ustun B, et al. Molecular characterization of pediatric gastrointestinal stromal tumors. Clin Cancer Res. 2008;14(10):3204-3215.
30. Janeway KA, Liegl B, Harlow A, et al. Pediatric KIT wild-type and platelet-derived growth factor receptor alpha-wild-type gastrointestinal stromal tumors share KIT activation but not mechanisms of genetic progression with adult gastrointestinal stromal tumors. Cancer Res. 2007;67(19):9084-9088.
31. Tarn C, Rink L, Merkel E, et al. Insulin-like growth factor 1 receptor is a potential therapeutic target for gastrointestinal stromal tumors. Proc Nat Acad Sci. 2008;105(24):8387-8392.
32. Stroobants S, Goeminne J, Seegers M, et al. 18FDG-Positron emission tomography for the early prediction of response in advanced soft tissue sarcoma treated with imatinib mesylate (Glivec). Eur J Cancer. 2003;39(14):2012-2020.
33. Antoch G, Kanja J, Bauer S, et al. Comparison of PET, CT, and dual-modality PET/CT imaging for monitoring of imatinib (STI571) therapy in patients with gastrointestinal stromal tumors. J Nuc Med. 2004;45(3):357-365.
34. Holdsworth CH, Badawi RD, Manola JB, et al. CT and PET: early prognostic indicators of response to imatinib mesylate in patients with gastrointestinal stromal tumor. Am J Roentgenol. 2007;189(6):W324-W330.
35. Choi H, Charnsangavej C, Faria SC, et al. Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol. 2007;25(13):1753-1759.
36. Le Cesne A, Ray-Coquard I, Bui BN, et al. Discontinuation of imatinib in patients with advanced gastrointestinal stromal tumours after 3 years of treatment: an open-label multicentre randomised phase 3 trial. Lancet Oncol. 2010;11(10):942-949.
37. Blay J-Y, Adenis A, Ray-Coquard I, Cassier PA, Le Cesne A. Is there a role for discontinuing imatinib in patients with advanced gastrointestinal stromal tumour? Curr Opin Oncol. 2009;21(4):360-366.
38. Casali PG, Jost L, Reichardt P, Schlemmer M, Blay JY; ESMO Guidelines Working Group. Gastrointestinal stromal tumors: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2008;19(suppl 2):ii35-ii38.
39. Sym SJ, Ryu MH, Lee JL, et al. Surgical intervention following imatinib treatment in patients with advanced gastrointestinal stromal tumors (GISTs). J Surg Oncol. 2008;98(1):27-33.
40. Al-Batran SE, Hartmann JT, Heidel F, et al. Focal progression in patients with gastrointestinal stromal tumors after initial response to imatinib mesylate: a three-center-based study of 38 patients. Gastric Cancer. 2007;10(3):145-152.
41. Haller F, Detken S, Schulten HJ, et al. Surgical management after neoadjuvant imatinib therapy in gastrointestinal stromal tumours (GISTs) with respect to imatinib resistance caused by secondary KIT mutations. Ann Surg Oncol. 2007;14(2):526-532.
42. Dematteo RP, Ballman KV, Antonescu CR, et al. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial.[Erratum appears in Lancet. 2009;374(9688):450]. Lancet. 2009;373(9669):1097-1104.
43. Corless C, Ballman KV, Antonescu C, et al. Relation of tumor pathologic and molecular features to outcome after surgical resection of localized primary gastrointestinal stromal tumor (GIST): results of the intergroup phase III trial ACOSOG Z9001 (abstract 10006). J Clin Oncol. 2010;28(suppl):15s.










